Duration of Treatment
usually takes 2 to 3 hours
Days of Stay
usually 2 to 4 days in the hospital and 5 days outside the hospital.
Anesthesia
General anaesthesia.
Cost
6000 TO 9000 USD
How much does Slipped Disc Surgery Cost in India?
"Looking for Slipped Disc Surgery Cost in India or Top Best Spine Hospitals at an affordable cost in different cities like Delhi, Mumbai, Chennai, Kolkata, and Bangalore? Here, we answer the question and explain how to choose the best spine surgeon for better results.
We have also shortlisted the list of best top Hospitals and Surgeons on the basis of Hospital accreditations, experience & qualification of surgeons, success rates of procedures, and patient testimonials.
- Slipped Disc Surgery Cost in India : Starting from 6,000 to 9,000 USD
- Hotel Cost Near Hospital - starting from 18 to 50 USD ( as per hotel services)
- Food Cost - starting from 20 to 30 USD (per day )
- Miscellaneous cost - 20 USD (per day)
- It's an only rough estimate, final treatment will plan after the fresh evaluation reports.
- In India, Slipped Disc Surgery Cost can vary as per the diagnosis, patient conditions, surgeon experience, Implant quality, hospital facilities, and city.
- To make an appointment, learn more about the slipped disc, read below information, or call / WhatsApp/ Viber - our experts to answer at +91 9582708782." Still, have questions? SUBMIT ENQUIRY
Who is the Top Best Spine Surgeon in India?
- Dr. Bipin Walia
- Dr. Rana Patir
- Dr. Anil Kumar Kansa
- Dr. Vikas Gupta
- Dr. Puneet Girdhar
- Dr. Saurabh Verma
- Dr. Aditya Gupta
- Dr. Sunit Mediratta
- Dr. Rahul Gupta
- Dr. Arun Saroha
- Dr. Anandh Balasubramaniam
- Dr. Shibu Vasudevan Pillai
Which is the best Slipped Disc Surgery Hospital in India?
- ARTEMIS HOSPITAL
- MANIPAL HOSPITAL
- BLK HOSPITAL
- APOLLO HOSPITAL
- FORTIS HOSPITAL
- MAX HOSPITAL
- MEDANTA HOSPITAL
- YASHODHA HOSPITAL
- GLOBAL HOSPITAL
- NARAYANA HOSPITAL
Why did you choose Peace Medical Tourism?
We are one of the best healthcare services providers for more than 10 years of experience to provide the best treatment at an affordable cost and guide our international patients to choose the top destination as per patient's budget and treatment.
- Comprehensive and 100% transparency.
- Help to Choose the Top Spine Hospitals in India.
- Very highly skilled Spine surgeon in India team.
- World-class technology for surgery.
- The high success rate of procedures with international standards.
- Affordable Cost of Best Slip Disc Surgery in india.
- best doctor for l4 l5 disc bulge.
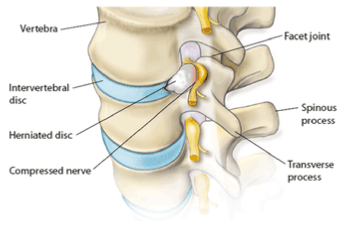
What is a Slipped Disc?
Slipped disc, also called a Spinal disc herniation, it refers to a complication of an intervertebral disc in the spine. These discs are rubbery cushions of cartilage acting as shock absorbers between the individual bones (vertebrae that comprise the spinal column. Disk removal is one of the most common types of spine surgery.
What are the types of slipped discs?
- Slipped cervical discs (Neck)
- Slipped thoracic discs (Upper body)
- Slipped lumbar discs (Lower back)
Still, have questions? SUBMIT ENQUIRY
What is the Signs and Symptoms of the Slipped disc?
- Pain and numbness
- Arms and legs pain
- Nerve root pain
- Pain when walking short distances
- Unexplained muscle weakness
- Tingling, aching, or burning sensations
What is the risk factor of Slipped disc surgery?
- Risks of anesthesia
- Bleeding
- Infection
- Leaking spinal fluid
- Bowel or bladder dysfunction
- Temporary dizziness
- Nerve paralysis
How to Prepare for Slipped Disc Surgery?
- First, you have to choose the best hospital for Spine surgery at an affordable cost for better results in India.
- The cost of Spine surgery starts from 7000 to 9000 USD depending upon the lung doctor’s experience, procedures, hospital facility, and city.
- The patient is required to go for PSC ( Pre-surgery check-up ) to do some blood test, ECG and ECH for Cardiac check-up and urine tests to know he /she is fit for surgery or not.
- Before the operation, you’ll be asked to sign a consent form, which gives the surgeon permission to carry out the treatment.
- The doctor should be informed about any medication that the patient may be taking.
- The patient is admitted to the hospital on the same days before the procedures and advised to remain empty stomach/Fasting.
- Thinners medicines have to stop before ten days of surgery.
How Slipped Disc Surgery Procedure Done?
Slipped disc surgery, also known as disc herniation surgery, is typically performed when conservative treatments like physical therapy, medication, or injections don't provide relief from pain or other symptoms. The procedure aims to remove the portion of the disc that is pressing on the spinal nerve, causing pain, numbness, or weakness. Here is an overview of how the surgery is done:
1. Preoperative Preparations:
- Anesthesia: The patient is usually given general anesthesia, meaning they will be asleep and pain-free during the procedure.
- Positioning: The patient is positioned on the operating table, typically lying on their stomach, so the surgeon can access the spine.
2. Incision:
- Minimally Invasive Approach: Surgeons may use a minimally invasive technique, which involves making a small incision, usually less than 2 inches long. A thin tube (retractor) is inserted through the incision to access the spine.
- Traditional Approach: In some cases, a larger incision may be made if the problem is more complex or if access is difficult with minimally invasive techniques.
3. Accessing the Disc:
- Removing Tissue: The surgeon carefully separates muscles and tissue to reach the spinal column and the affected disc.
- Removal of Herniated Portion: The disc that has slipped out of place is identified. The herniated (protruding) portion of the disc is then carefully removed to relieve the pressure on the spinal nerves.
4. Disc Decompression:
- Relieving Nerve Pressure: The surgeon may remove part of the disc or the entire disc to relieve the pressure causing pain, numbness, or weakness.
- Bone Spur Removal: If bone spurs or fragments from the disc are pressing on the nerves, they are also removed to further decompress the area.
5. Stabilization (if necessary):
- Fusion Surgery: In some cases, the surgeon may perform a spinal fusion to stabilize the spine after the disc is removed. This involves joining two vertebrae together using bone grafts or implants.
- Artificial Disc Replacement: In some cases, the surgeon may replace the damaged disc with an artificial disc to maintain motion in the spine.
6. Closing the Incision:
- After the disc material is removed and the area is cleared of debris, the surgeon closes the incision with sutures or staples.
- Dressing: A sterile dressing is applied to the wound.
7. Postoperative Care:
- Recovery: After surgery, the patient may be observed for a few hours in the recovery room. Pain management is provided to control discomfort.
- Rehabilitation: The patient will likely need physical therapy to regain strength and mobility. The recovery period can vary, but many people experience relief from symptoms within weeks to months.
Types of Surgery for Slipped Disc:
- Discectomy: Removal of the herniated disc material.
- Laminectomy: Removal of part of the vertebra (lamina) to relieve pressure on the spinal nerves.
- Spinal Fusion: Fusing two or more vertebrae to provide stability to the spine.
- Artificial Disc Replacement: Replacing the damaged disc with an artificial one to maintain spine flexibility.
Risks and Recovery:
- Risks: As with any surgery, there are risks of infection, bleeding, nerve damage, or complications related to anesthesia.
- Recovery: Recovery times can vary depending on the type of surgery performed, but many patients begin walking within a day or two and gradually return to normal activities within weeks.
Surgical intervention for a slipped disc is generally considered a last resort after other treatments have been exhausted, but when necessary, it can significantly improve quality of life by reducing pain and nerve-related symptoms.
What is the Post Care for Slipped Disc Surgery?
Post-operative care for slipped disc surgery is crucial for ensuring a smooth recovery, minimizing complications, and enhancing the overall success of the surgery. Below are the key aspects of post-care following slipped disc surgery:
1. Immediate Post-Operative Care:
- Recovery Room: After surgery, patients are taken to the recovery room where medical staff monitor their vital signs, including heart rate, blood pressure, and oxygen levels.
- Pain Management: Pain relief is managed with medications, typically including opioids in the short term, as well as non-steroidal anti-inflammatory drugs (NSAIDs) to reduce inflammation. Patients are encouraged to report any significant pain or discomfort.
- Antibiotics: If the surgeon has prescribed antibiotics, they are administered to prevent infection.
- Wound Care: The surgical site is typically covered with a sterile dressing. Nurses will monitor the wound for signs of infection, and it may be changed regularly.
2. Mobility and Activity:
- Gradual Movement: Depending on the surgery type (e.g., minimally invasive or traditional), patients may be encouraged to start moving, sitting, or walking with assistance within a few hours of surgery. This helps prevent complications such as blood clots or muscle stiffness.
- Walking: Light walking is encouraged within 1-2 days after surgery. Patients should avoid prolonged bed rest as it may slow down recovery.
- Avoid Lifting and Straining: Heavy lifting, bending, or twisting should be avoided, particularly in the first few weeks. These activities can strain the spine and impede healing.
- Bracing: In some cases, the surgeon may recommend a back brace to help stabilize the spine during the recovery period.
3. Pain Management:
- Post-Op Pain: It’s normal to experience some pain or discomfort after surgery. Pain management may involve a combination of oral pain medications, ice packs, and possibly muscle relaxants.
- Weaning off Painkillers: Over time, the use of prescription painkillers will be reduced, and patients may transition to over-the-counter pain relievers like acetaminophen or ibuprofen.
4. Physical Therapy and Rehabilitation:
- Physical Therapy: Most patients will begin physical therapy 1-2 weeks after surgery, depending on their recovery progress. Physical therapy helps improve flexibility, strengthen core muscles, and reduce the risk of re-injury.
- Stretching and Strengthening: Gradually, patients are taught exercises to improve spinal mobility and overall posture. These exercises will also focus on strengthening muscles around the spine to support it during recovery.
- Posture Correction: Patients may be instructed on how to maintain proper posture during daily activities, which is essential for avoiding undue stress on the back during recovery.
5. Follow-Up Appointments:
- Surgical Site Inspection: The surgeon will likely schedule follow-up visits to check the healing process of the surgical site and remove sutures or staples, if necessary.
- Imaging: In some cases, imaging tests like X-rays or MRIs may be used to confirm that the disc is healing well and that there are no complications.
6. Diet and Hydration:
- Healthy Diet: A balanced diet rich in vitamins, minerals, and protein is recommended to support the healing process. Patients may be advised to include foods that promote bone health (e.g., calcium and vitamin D).
- Hydration: Keeping hydrated is important to ensure good circulation and overall health during recovery.
7. Signs of Complications:
Patients should be aware of potential complications and seek medical attention if they experience:
- Increased pain or swelling at the surgical site.
- Signs of infection such as redness, warmth, or discharge from the wound.
- Fever or chills.
- Changes in bowel or bladder function, including incontinence or difficulty urinating, which may indicate nerve involvement.
- Leg weakness or numbness, which may suggest a recurrence of nerve compression.
- Deep vein thrombosis (DVT) signs, like swelling, redness, or pain in the legs.
8. Lifestyle Modifications and Long-Term Care:
- Weight Management: Maintaining a healthy weight is important to reduce the strain on the spine.
- Ergonomic Adjustments: Adjusting work and home environments to reduce strain on the back, such as using ergonomic furniture, can help prevent re-injury.
- Gradual Return to Normal Activities: Patients are usually advised to gradually resume normal activities, with full return to work or more strenuous exercises often taking 6-8 weeks, depending on the nature of the surgery and individual healing progress.
9. Avoiding Smoking and Alcohol:
- Smoking: Smoking can delay healing, so it's advisable to stop smoking before and after surgery.
- Alcohol: Excessive alcohol consumption can impair the healing process, and it’s best to avoid drinking alcohol during the recovery period.
10. Time to Full Recovery:
- Recovery time varies based on the type of surgery and individual health. Typically, patients can expect a recovery period of 6-12 weeks for most activities. However, full recovery, particularly from more complex surgeries, may take up to 6 months or longer.
- Ongoing therapy and exercise during recovery are crucial for restoring mobility and strength.
By closely following post-operative care instructions and making lifestyle adjustments, patients can enhance their recovery, reduce the risk of complications, and ultimately return to a pain-free, active life.
What is the Success rate of Slipped Disc Surgery in India?
The success rate of slipped disc surgery in India is generally high, ranging from 80% to 95%, depending on factors like the type of surgery, the patient's overall health, the severity of the condition, and the skill of the surgeon. Here are some insights into the factors that influence the success rate:
1. Type of Surgery:
- Discectomy (Removal of Herniated Disc): This is the most common surgery for a slipped disc, and the success rate is usually high. Studies suggest that 80% to 90% of patients experience significant pain relief and improvement in mobility after the surgery.
- Minimally Invasive Surgery: This technique typically leads to quicker recovery, less pain, and fewer complications. Success rates for minimally invasive procedures are also comparable, with many patients reporting improved quality of life post-surgery.
- Spinal Fusion: If fusion is required due to disc removal or instability in the spine, the success rate can be slightly lower, but many patients achieve good outcomes in terms of pain relief and spinal stability. Success rates for spinal fusion surgeries are usually around 85% to 90%.
- Artificial Disc Replacement: For cases where an artificial disc is used, the success rate is similar to that of discectomy and spinal fusion, with many patients experiencing long-term relief from pain and better functionality.
2. Factors Affecting Success:
- Timeliness of Surgery: Early intervention generally results in better outcomes. Surgery done within a few months of symptom onset, especially in cases of nerve compression, can help improve the success rate.
- Patient Health: Patients who are in good general health and maintain a healthy weight tend to recover more quickly and experience better results.
- Age and Activity Level: Younger patients and those who have an active lifestyle tend to have faster recovery times and more successful outcomes. Older adults or those with chronic health issues may experience slower recovery or complications.
- Post-Surgery Rehabilitation: Adherence to post-operative care, including physical therapy and lifestyle modifications, is crucial for achieving the best outcome.
3. Indian Healthcare Context:
- India has a large number of highly experienced spine surgeons and specialized spinal surgery centers in cities like Delhi, Mumbai, Bengaluru, and Chennai, which have contributed to high success rates. Many of these centers use state-of-the-art medical equipment and advanced techniques like robotic-assisted spine surgery, which further enhance the success rates.
- Additionally, the cost-effectiveness of surgery in India compared to other countries does not compromise the quality of care, contributing to better access to treatment and timely interventions.
4. Patient Satisfaction and Long-Term Results:
- A significant number of patients report a reduction in pain, increased mobility, and an improved quality of life after slipped disc surgery in India. The long-term success rate remains high for most individuals, especially when they follow post-operative care instructions and incorporate rehabilitation practices into their recovery.
5. Complications and Risks:
- While the success rates are high, like all surgeries, there are potential risks, such as infection, nerve damage, or recurrence of disc herniation. However, these complications are relatively rare, especially when surgery is performed by skilled surgeons in accredited hospitals.
In conclusion, the success rate of slipped disc surgery in India is quite favorable, making it an excellent option for those considering spine surgery. With the availability of world-class hospitals, experienced surgeons, and modern surgical techniques, patients can expect to achieve substantial relief from symptoms and resume normal activities with a high degree of success.
What Questions Ask before Slipped Disc Surgery?
1. Is Surgery the Right Option for Me?
-
Why do you recommend surgery over other treatments? Surgery is recommended when conservative treatments (such as physical therapy, medication, or epidural injections) fail to alleviate symptoms, especially if the slipped disc is causing severe pain, weakness, or nerve damage. Surgery is typically considered when the symptoms are significantly impacting your daily life and quality of life.
-
What are the risks of delaying surgery versus having it now? Delaying surgery could potentially lead to further nerve damage, muscle weakness, or long-term complications like permanent disability. The condition could worsen over time, making recovery more difficult after a prolonged delay.
-
What non-surgical treatments have I already tried, and why were they not effective? Non-surgical treatments like pain medications, physical therapy, and spinal injections are usually effective for less severe cases. However, they may not work if the herniated disc is large, pressing on nerves, or causing irreversible damage. Surgery may be necessary if these methods fail to address the root cause of your symptoms.
2. What Type of Surgery Do You Recommend?
-
What kind of surgery will I undergo (discectomy, spinal fusion, minimally invasive, artificial disc replacement)? Based on your condition, I may recommend a discectomy, where the herniated portion of the disc is removed. If there is significant spinal instability, I may recommend spinal fusion, where two or more vertebrae are fused together. Alternatively, minimally invasive surgery might be an option for quicker recovery with smaller incisions. In some cases, artificial disc replacement is recommended to restore the function of the disc.
-
Why do you recommend this specific type of surgery for my condition? The recommended surgery is chosen based on factors like the size and location of the herniated disc, your age, overall health, and the extent of nerve compression. For example, if you have a large herniation that’s causing nerve damage, a discectomy may be the best option.
-
Are there alternative surgeries or techniques I should consider? Alternative options could include artificial disc replacement or a minimally invasive procedure if you have a specific type of disc herniation or if your spine is still relatively healthy and doesn’t require fusion.
3. What Are the Risks and Complications?
-
What are the potential risks and complications associated with this surgery? Risks include infection, bleeding, nerve damage, blood clots, and spinal instability. While rare, complications can also include persistent pain or worsening of symptoms.
-
How common are complications like infection, nerve damage, or spinal instability? Infection and nerve damage are rare, occurring in less than 1% of surgeries. Spinal instability is more common if multiple vertebrae are involved, but this is still relatively uncommon.
-
What are the signs of complications I should watch out for after the surgery? Watch for symptoms like fever, increased pain, swelling, redness at the incision site, numbness, tingling, or difficulty moving. Any changes in bowel or bladder control should be reported immediately as this could indicate nerve compression.
4. What is the Expected Outcome?
-
What are the chances of complete pain relief or improvement in symptoms after surgery? There is a high likelihood of pain relief and symptom improvement, with most patients reporting significant improvement or complete resolution of symptoms. Success rates range from 80% to 95% depending on the severity and type of surgery.
-
What is the typical recovery time for this surgery? The typical recovery time varies, but you can expect to resume light activities in 2 to 6 weeks, and full recovery can take up to 3 to 6 months, depending on the complexity of the surgery.
-
Will I need follow-up treatments, like physical therapy or additional surgeries? Physical therapy is often recommended to strengthen muscles around the spine and improve flexibility. Additional surgery is rare but may be necessary if the disc herniation recurs or if complications arise.
-
Is there a possibility that the herniated disc could recur? Yes, though the recurrence rate is low, especially if post-operative care and lifestyle modifications are followed.
5. What is the Success Rate of This Surgery?
-
What is the success rate for this surgery, particularly for my type of disc herniation? The success rate is generally high, around 80% to 95%, for relieving symptoms such as pain and numbness. The rate may vary depending on the type of surgery and individual factors.
-
How many similar surgeries have you performed, and what is your experience with this procedure? I have performed over [insert number] surgeries and have experience with various techniques, including minimally invasive procedures and complex cases.
-
What are the long-term outcomes for patients who undergo this surgery? Most patients experience long-term relief from symptoms, with many able to return to normal activities. However, maintaining good spine health through proper posture and exercise is essential.
6. What Will My Recovery Be Like?
-
What is the expected recovery time, and when can I resume normal activities (work, exercise, driving)? The recovery time varies, but light activities like walking may be resumed within a few days to a week, while more strenuous activities and work can be resumed in 4 to 6 weeks. Driving may be possible in about 2 to 4 weeks, depending on pain levels and mobility.
-
Will I need to stay in the hospital after surgery, and if so, for how long? You may stay in the hospital for 1 to 2 days for monitoring, depending on the surgery’s complexity and your recovery progress.
-
Will I need assistance at home during the recovery period? You may need help with daily tasks for the first week or two, especially if mobility is limited.
-
What activities should I avoid during recovery, and when can I return to physical activities or sports? Avoid heavy lifting, bending, or twisting for 4 to 6 weeks. Full participation in physical activities and sports may be possible in 3 to 6 months after completing physical therapy.
-
What kind of rehabilitation or physical therapy will I need post-surgery? A rehabilitation program focusing on strengthening the muscles around the spine, improving flexibility, and promoting healthy posture will be recommended.
7. What Should I Expect in Terms of Pain After Surgery?
-
How much pain or discomfort should I expect after the surgery? Mild to moderate pain is common in the initial post-operative period, but this should improve within a few weeks. The pain should be manageable with prescribed medications.
-
What pain management options are available, and for how long will I need them? Pain management may include prescription painkillers in the early stages, followed by over-the-counter medications like ibuprofen. Most patients can stop using pain medications after a few weeks.
-
Are there alternative methods to manage pain (e.g., ice packs, medications, relaxation techniques)? Ice packs, physical therapy, and relaxation techniques such as deep breathing or meditation can also help manage pain.
8. What Are the Costs and Insurance Coverage?
-
What is the total cost of the surgery, including pre-operative tests, the surgery itself, and post-operative care? The total cost can range between [insert cost range] depending on the hospital, location, and specific procedure.
-
Does my insurance cover the procedure, and if not, what are my financing options? Most insurance plans cover the procedure, but it’s best to confirm with your provider. Financing options may be available if needed.
-
Are there any hidden costs or additional charges I should be aware of? Be sure to ask about the cost of pre-operative tests, medications, and physical therapy that may not be covered by insurance.
9. What Happens If Surgery Does Not Work?
- What if the surgery does not relieve my symptoms or if the problem recurs? In rare cases, further surgery or alternative treatments may be required. We can explore options like additional spinal procedures or therapies.
10. What Are the Pre-Operative Instructions?
-
What do I need to do before surgery to prepare (e.g., fasting, medications to stop, or supplements to avoid)? Typically, you will need to fast for at least 6 hours before surgery and avoid certain medications like blood thinners or anti-inflammatory drugs.
-
Do I need to stop any medications or supplements before surgery, and how will that affect my health? Some medications, such as blood thinners, may need to be paused. Consult with your doctor about the medications you are currently taking.
-
Are there any lifestyle changes (e.g., stopping smoking or weight management) I should make before surgery to improve my outcomes? Smoking cessation and maintaining a healthy weight can significantly improve recovery outcomes.
11. Who Will Perform the Surgery, and How Experienced Are They?
-
Will the same surgeon who is consulting with me perform the surgery? Yes, I will be performing your surgery personally, and I have extensive experience with this procedure.
-
How many of these surgeries have you performed, and what is your success rate? I have performed [insert number] surgeries with a success rate of [insert success rate].
-
Will a surgical team assist, and what is their level of expertise? Yes, a skilled surgical team will assist, and each member has expertise in spinal surgeries.
12. Post-Operative Care and Follow-Up:
-
What post-operative care will I need, and how frequently will I need to follow up with you? Follow-up visits will be scheduled for the first few months to monitor healing and discuss physical therapy.
-
What kind of support or guidance will be available if I have concerns after surgery? A dedicated support team will be available for any questions or concerns, and I will be available for emergency consultation if necessary.
This comprehensive list of questions and answers will help you get the information you need before making an informed decision about your surgery.
Top Doctors
Top Hospitals
SLIPPED DISC SURGERY COST IN INDIA
Duration of Treatment
usually takes 2 to 3 hours
Days of Stay
usually 2 to 4 days in the hospital and 5 days outside the hospital.
Anesthesia
General anaesthesia.
Cost
6000 TO 9000 USD
How much does Slipped Disc Surgery Cost in India?
"Looking for Slipped Disc Surgery Cost in India or Top Best Spine Hospitals at an affordable cost in different cities like Delhi, Mumbai, Chennai, Kolkata, and Bangalore? Here, we answer the question and explain how to choose the best spine surgeon for better results.
We have also shortlisted the list of best top Hospitals and Surgeons on the basis of Hospital accreditations, experience & qualification of surgeons, success rates of procedures, and patient testimonials.
- Slipped Disc Surgery Cost in India : Starting from 6,000 to 9,000 USD
- Hotel Cost Near Hospital - starting from 18 to 50 USD ( as per hotel services)
- Food Cost - starting from 20 to 30 USD (per day )
- Miscellaneous cost - 20 USD (per day)
- It's an only rough estimate, final treatment will plan after the fresh evaluation reports.
- In India, Slipped Disc Surgery Cost can vary as per the diagnosis, patient conditions, surgeon experience, Implant quality, hospital facilities, and city.
- To make an appointment, learn more about the slipped disc, read below information, or call / WhatsApp/ Viber - our experts to answer at +91 9582708782." Still, have questions? SUBMIT ENQUIRY
Who is the Top Best Spine Surgeon in India?
- Dr. Bipin Walia
- Dr. Rana Patir
- Dr. Anil Kumar Kansa
- Dr. Vikas Gupta
- Dr. Puneet Girdhar
- Dr. Saurabh Verma
- Dr. Aditya Gupta
- Dr. Sunit Mediratta
- Dr. Rahul Gupta
- Dr. Arun Saroha
- Dr. Anandh Balasubramaniam
- Dr. Shibu Vasudevan Pillai
Which is the best Slipped Disc Surgery Hospital in India?
- ARTEMIS HOSPITAL
- MANIPAL HOSPITAL
- BLK HOSPITAL
- APOLLO HOSPITAL
- FORTIS HOSPITAL
- MAX HOSPITAL
- MEDANTA HOSPITAL
- YASHODHA HOSPITAL
- GLOBAL HOSPITAL
- NARAYANA HOSPITAL
Why did you choose Peace Medical Tourism?
We are one of the best healthcare services providers for more than 10 years of experience to provide the best treatment at an affordable cost and guide our international patients to choose the top destination as per patient's budget and treatment.
- Comprehensive and 100% transparency.
- Help to Choose the Top Spine Hospitals in India.
- Very highly skilled Spine surgeon in India team.
- World-class technology for surgery.
- The high success rate of procedures with international standards.
- Affordable Cost of Best Slip Disc Surgery in india.
- best doctor for l4 l5 disc bulge.
What is a Slipped Disc?
Slipped disc, also called a Spinal disc herniation, it refers to a complication of an intervertebral disc in the spine. These discs are rubbery cushions of cartilage acting as shock absorbers between the individual bones (vertebrae that comprise the spinal column. Disk removal is one of the most common types of spine surgery.
What are the types of slipped discs?
- Slipped cervical discs (Neck)
- Slipped thoracic discs (Upper body)
- Slipped lumbar discs (Lower back)
Still, have questions? SUBMIT ENQUIRY
symptoms
What is the Signs and Symptoms of the Slipped disc?
- Pain and numbness
- Arms and legs pain
- Nerve root pain
- Pain when walking short distances
- Unexplained muscle weakness
- Tingling, aching, or burning sensations
risk factors
What is the risk factor of Slipped disc surgery?
- Risks of anesthesia
- Bleeding
- Infection
- Leaking spinal fluid
- Bowel or bladder dysfunction
- Temporary dizziness
- Nerve paralysis
preparation
How to Prepare for Slipped Disc Surgery?
- First, you have to choose the best hospital for Spine surgery at an affordable cost for better results in India.
- The cost of Spine surgery starts from 7000 to 9000 USD depending upon the lung doctor’s experience, procedures, hospital facility, and city.
- The patient is required to go for PSC ( Pre-surgery check-up ) to do some blood test, ECG and ECH for Cardiac check-up and urine tests to know he /she is fit for surgery or not.
- Before the operation, you’ll be asked to sign a consent form, which gives the surgeon permission to carry out the treatment.
- The doctor should be informed about any medication that the patient may be taking.
- The patient is admitted to the hospital on the same days before the procedures and advised to remain empty stomach/Fasting.
- Thinners medicines have to stop before ten days of surgery.
procedure
How Slipped Disc Surgery Procedure Done?
Slipped disc surgery, also known as disc herniation surgery, is typically performed when conservative treatments like physical therapy, medication, or injections don't provide relief from pain or other symptoms. The procedure aims to remove the portion of the disc that is pressing on the spinal nerve, causing pain, numbness, or weakness. Here is an overview of how the surgery is done:
1. Preoperative Preparations:
- Anesthesia: The patient is usually given general anesthesia, meaning they will be asleep and pain-free during the procedure.
- Positioning: The patient is positioned on the operating table, typically lying on their stomach, so the surgeon can access the spine.
2. Incision:
- Minimally Invasive Approach: Surgeons may use a minimally invasive technique, which involves making a small incision, usually less than 2 inches long. A thin tube (retractor) is inserted through the incision to access the spine.
- Traditional Approach: In some cases, a larger incision may be made if the problem is more complex or if access is difficult with minimally invasive techniques.
3. Accessing the Disc:
- Removing Tissue: The surgeon carefully separates muscles and tissue to reach the spinal column and the affected disc.
- Removal of Herniated Portion: The disc that has slipped out of place is identified. The herniated (protruding) portion of the disc is then carefully removed to relieve the pressure on the spinal nerves.
4. Disc Decompression:
- Relieving Nerve Pressure: The surgeon may remove part of the disc or the entire disc to relieve the pressure causing pain, numbness, or weakness.
- Bone Spur Removal: If bone spurs or fragments from the disc are pressing on the nerves, they are also removed to further decompress the area.
5. Stabilization (if necessary):
- Fusion Surgery: In some cases, the surgeon may perform a spinal fusion to stabilize the spine after the disc is removed. This involves joining two vertebrae together using bone grafts or implants.
- Artificial Disc Replacement: In some cases, the surgeon may replace the damaged disc with an artificial disc to maintain motion in the spine.
6. Closing the Incision:
- After the disc material is removed and the area is cleared of debris, the surgeon closes the incision with sutures or staples.
- Dressing: A sterile dressing is applied to the wound.
7. Postoperative Care:
- Recovery: After surgery, the patient may be observed for a few hours in the recovery room. Pain management is provided to control discomfort.
- Rehabilitation: The patient will likely need physical therapy to regain strength and mobility. The recovery period can vary, but many people experience relief from symptoms within weeks to months.
Types of Surgery for Slipped Disc:
- Discectomy: Removal of the herniated disc material.
- Laminectomy: Removal of part of the vertebra (lamina) to relieve pressure on the spinal nerves.
- Spinal Fusion: Fusing two or more vertebrae to provide stability to the spine.
- Artificial Disc Replacement: Replacing the damaged disc with an artificial one to maintain spine flexibility.
Risks and Recovery:
- Risks: As with any surgery, there are risks of infection, bleeding, nerve damage, or complications related to anesthesia.
- Recovery: Recovery times can vary depending on the type of surgery performed, but many patients begin walking within a day or two and gradually return to normal activities within weeks.
Surgical intervention for a slipped disc is generally considered a last resort after other treatments have been exhausted, but when necessary, it can significantly improve quality of life by reducing pain and nerve-related symptoms.
post procedure
What is the Post Care for Slipped Disc Surgery?
Post-operative care for slipped disc surgery is crucial for ensuring a smooth recovery, minimizing complications, and enhancing the overall success of the surgery. Below are the key aspects of post-care following slipped disc surgery:
1. Immediate Post-Operative Care:
- Recovery Room: After surgery, patients are taken to the recovery room where medical staff monitor their vital signs, including heart rate, blood pressure, and oxygen levels.
- Pain Management: Pain relief is managed with medications, typically including opioids in the short term, as well as non-steroidal anti-inflammatory drugs (NSAIDs) to reduce inflammation. Patients are encouraged to report any significant pain or discomfort.
- Antibiotics: If the surgeon has prescribed antibiotics, they are administered to prevent infection.
- Wound Care: The surgical site is typically covered with a sterile dressing. Nurses will monitor the wound for signs of infection, and it may be changed regularly.
2. Mobility and Activity:
- Gradual Movement: Depending on the surgery type (e.g., minimally invasive or traditional), patients may be encouraged to start moving, sitting, or walking with assistance within a few hours of surgery. This helps prevent complications such as blood clots or muscle stiffness.
- Walking: Light walking is encouraged within 1-2 days after surgery. Patients should avoid prolonged bed rest as it may slow down recovery.
- Avoid Lifting and Straining: Heavy lifting, bending, or twisting should be avoided, particularly in the first few weeks. These activities can strain the spine and impede healing.
- Bracing: In some cases, the surgeon may recommend a back brace to help stabilize the spine during the recovery period.
3. Pain Management:
- Post-Op Pain: It’s normal to experience some pain or discomfort after surgery. Pain management may involve a combination of oral pain medications, ice packs, and possibly muscle relaxants.
- Weaning off Painkillers: Over time, the use of prescription painkillers will be reduced, and patients may transition to over-the-counter pain relievers like acetaminophen or ibuprofen.
4. Physical Therapy and Rehabilitation:
- Physical Therapy: Most patients will begin physical therapy 1-2 weeks after surgery, depending on their recovery progress. Physical therapy helps improve flexibility, strengthen core muscles, and reduce the risk of re-injury.
- Stretching and Strengthening: Gradually, patients are taught exercises to improve spinal mobility and overall posture. These exercises will also focus on strengthening muscles around the spine to support it during recovery.
- Posture Correction: Patients may be instructed on how to maintain proper posture during daily activities, which is essential for avoiding undue stress on the back during recovery.
5. Follow-Up Appointments:
- Surgical Site Inspection: The surgeon will likely schedule follow-up visits to check the healing process of the surgical site and remove sutures or staples, if necessary.
- Imaging: In some cases, imaging tests like X-rays or MRIs may be used to confirm that the disc is healing well and that there are no complications.
6. Diet and Hydration:
- Healthy Diet: A balanced diet rich in vitamins, minerals, and protein is recommended to support the healing process. Patients may be advised to include foods that promote bone health (e.g., calcium and vitamin D).
- Hydration: Keeping hydrated is important to ensure good circulation and overall health during recovery.
7. Signs of Complications:
Patients should be aware of potential complications and seek medical attention if they experience:
- Increased pain or swelling at the surgical site.
- Signs of infection such as redness, warmth, or discharge from the wound.
- Fever or chills.
- Changes in bowel or bladder function, including incontinence or difficulty urinating, which may indicate nerve involvement.
- Leg weakness or numbness, which may suggest a recurrence of nerve compression.
- Deep vein thrombosis (DVT) signs, like swelling, redness, or pain in the legs.
8. Lifestyle Modifications and Long-Term Care:
- Weight Management: Maintaining a healthy weight is important to reduce the strain on the spine.
- Ergonomic Adjustments: Adjusting work and home environments to reduce strain on the back, such as using ergonomic furniture, can help prevent re-injury.
- Gradual Return to Normal Activities: Patients are usually advised to gradually resume normal activities, with full return to work or more strenuous exercises often taking 6-8 weeks, depending on the nature of the surgery and individual healing progress.
9. Avoiding Smoking and Alcohol:
- Smoking: Smoking can delay healing, so it's advisable to stop smoking before and after surgery.
- Alcohol: Excessive alcohol consumption can impair the healing process, and it’s best to avoid drinking alcohol during the recovery period.
10. Time to Full Recovery:
- Recovery time varies based on the type of surgery and individual health. Typically, patients can expect a recovery period of 6-12 weeks for most activities. However, full recovery, particularly from more complex surgeries, may take up to 6 months or longer.
- Ongoing therapy and exercise during recovery are crucial for restoring mobility and strength.
By closely following post-operative care instructions and making lifestyle adjustments, patients can enhance their recovery, reduce the risk of complications, and ultimately return to a pain-free, active life.
success rate
What is the Success rate of Slipped Disc Surgery in India?
The success rate of slipped disc surgery in India is generally high, ranging from 80% to 95%, depending on factors like the type of surgery, the patient's overall health, the severity of the condition, and the skill of the surgeon. Here are some insights into the factors that influence the success rate:
1. Type of Surgery:
- Discectomy (Removal of Herniated Disc): This is the most common surgery for a slipped disc, and the success rate is usually high. Studies suggest that 80% to 90% of patients experience significant pain relief and improvement in mobility after the surgery.
- Minimally Invasive Surgery: This technique typically leads to quicker recovery, less pain, and fewer complications. Success rates for minimally invasive procedures are also comparable, with many patients reporting improved quality of life post-surgery.
- Spinal Fusion: If fusion is required due to disc removal or instability in the spine, the success rate can be slightly lower, but many patients achieve good outcomes in terms of pain relief and spinal stability. Success rates for spinal fusion surgeries are usually around 85% to 90%.
- Artificial Disc Replacement: For cases where an artificial disc is used, the success rate is similar to that of discectomy and spinal fusion, with many patients experiencing long-term relief from pain and better functionality.
2. Factors Affecting Success:
- Timeliness of Surgery: Early intervention generally results in better outcomes. Surgery done within a few months of symptom onset, especially in cases of nerve compression, can help improve the success rate.
- Patient Health: Patients who are in good general health and maintain a healthy weight tend to recover more quickly and experience better results.
- Age and Activity Level: Younger patients and those who have an active lifestyle tend to have faster recovery times and more successful outcomes. Older adults or those with chronic health issues may experience slower recovery or complications.
- Post-Surgery Rehabilitation: Adherence to post-operative care, including physical therapy and lifestyle modifications, is crucial for achieving the best outcome.
3. Indian Healthcare Context:
- India has a large number of highly experienced spine surgeons and specialized spinal surgery centers in cities like Delhi, Mumbai, Bengaluru, and Chennai, which have contributed to high success rates. Many of these centers use state-of-the-art medical equipment and advanced techniques like robotic-assisted spine surgery, which further enhance the success rates.
- Additionally, the cost-effectiveness of surgery in India compared to other countries does not compromise the quality of care, contributing to better access to treatment and timely interventions.
4. Patient Satisfaction and Long-Term Results:
- A significant number of patients report a reduction in pain, increased mobility, and an improved quality of life after slipped disc surgery in India. The long-term success rate remains high for most individuals, especially when they follow post-operative care instructions and incorporate rehabilitation practices into their recovery.
5. Complications and Risks:
- While the success rates are high, like all surgeries, there are potential risks, such as infection, nerve damage, or recurrence of disc herniation. However, these complications are relatively rare, especially when surgery is performed by skilled surgeons in accredited hospitals.
In conclusion, the success rate of slipped disc surgery in India is quite favorable, making it an excellent option for those considering spine surgery. With the availability of world-class hospitals, experienced surgeons, and modern surgical techniques, patients can expect to achieve substantial relief from symptoms and resume normal activities with a high degree of success.
faqs from doctor
What Questions Ask before Slipped Disc Surgery?
1. Is Surgery the Right Option for Me?
-
Why do you recommend surgery over other treatments? Surgery is recommended when conservative treatments (such as physical therapy, medication, or epidural injections) fail to alleviate symptoms, especially if the slipped disc is causing severe pain, weakness, or nerve damage. Surgery is typically considered when the symptoms are significantly impacting your daily life and quality of life.
-
What are the risks of delaying surgery versus having it now? Delaying surgery could potentially lead to further nerve damage, muscle weakness, or long-term complications like permanent disability. The condition could worsen over time, making recovery more difficult after a prolonged delay.
-
What non-surgical treatments have I already tried, and why were they not effective? Non-surgical treatments like pain medications, physical therapy, and spinal injections are usually effective for less severe cases. However, they may not work if the herniated disc is large, pressing on nerves, or causing irreversible damage. Surgery may be necessary if these methods fail to address the root cause of your symptoms.
2. What Type of Surgery Do You Recommend?
-
What kind of surgery will I undergo (discectomy, spinal fusion, minimally invasive, artificial disc replacement)? Based on your condition, I may recommend a discectomy, where the herniated portion of the disc is removed. If there is significant spinal instability, I may recommend spinal fusion, where two or more vertebrae are fused together. Alternatively, minimally invasive surgery might be an option for quicker recovery with smaller incisions. In some cases, artificial disc replacement is recommended to restore the function of the disc.
-
Why do you recommend this specific type of surgery for my condition? The recommended surgery is chosen based on factors like the size and location of the herniated disc, your age, overall health, and the extent of nerve compression. For example, if you have a large herniation that’s causing nerve damage, a discectomy may be the best option.
-
Are there alternative surgeries or techniques I should consider? Alternative options could include artificial disc replacement or a minimally invasive procedure if you have a specific type of disc herniation or if your spine is still relatively healthy and doesn’t require fusion.
3. What Are the Risks and Complications?
-
What are the potential risks and complications associated with this surgery? Risks include infection, bleeding, nerve damage, blood clots, and spinal instability. While rare, complications can also include persistent pain or worsening of symptoms.
-
How common are complications like infection, nerve damage, or spinal instability? Infection and nerve damage are rare, occurring in less than 1% of surgeries. Spinal instability is more common if multiple vertebrae are involved, but this is still relatively uncommon.
-
What are the signs of complications I should watch out for after the surgery? Watch for symptoms like fever, increased pain, swelling, redness at the incision site, numbness, tingling, or difficulty moving. Any changes in bowel or bladder control should be reported immediately as this could indicate nerve compression.
4. What is the Expected Outcome?
-
What are the chances of complete pain relief or improvement in symptoms after surgery? There is a high likelihood of pain relief and symptom improvement, with most patients reporting significant improvement or complete resolution of symptoms. Success rates range from 80% to 95% depending on the severity and type of surgery.
-
What is the typical recovery time for this surgery? The typical recovery time varies, but you can expect to resume light activities in 2 to 6 weeks, and full recovery can take up to 3 to 6 months, depending on the complexity of the surgery.
-
Will I need follow-up treatments, like physical therapy or additional surgeries? Physical therapy is often recommended to strengthen muscles around the spine and improve flexibility. Additional surgery is rare but may be necessary if the disc herniation recurs or if complications arise.
-
Is there a possibility that the herniated disc could recur? Yes, though the recurrence rate is low, especially if post-operative care and lifestyle modifications are followed.
5. What is the Success Rate of This Surgery?
-
What is the success rate for this surgery, particularly for my type of disc herniation? The success rate is generally high, around 80% to 95%, for relieving symptoms such as pain and numbness. The rate may vary depending on the type of surgery and individual factors.
-
How many similar surgeries have you performed, and what is your experience with this procedure? I have performed over [insert number] surgeries and have experience with various techniques, including minimally invasive procedures and complex cases.
-
What are the long-term outcomes for patients who undergo this surgery? Most patients experience long-term relief from symptoms, with many able to return to normal activities. However, maintaining good spine health through proper posture and exercise is essential.
6. What Will My Recovery Be Like?
-
What is the expected recovery time, and when can I resume normal activities (work, exercise, driving)? The recovery time varies, but light activities like walking may be resumed within a few days to a week, while more strenuous activities and work can be resumed in 4 to 6 weeks. Driving may be possible in about 2 to 4 weeks, depending on pain levels and mobility.
-
Will I need to stay in the hospital after surgery, and if so, for how long? You may stay in the hospital for 1 to 2 days for monitoring, depending on the surgery’s complexity and your recovery progress.
-
Will I need assistance at home during the recovery period? You may need help with daily tasks for the first week or two, especially if mobility is limited.
-
What activities should I avoid during recovery, and when can I return to physical activities or sports? Avoid heavy lifting, bending, or twisting for 4 to 6 weeks. Full participation in physical activities and sports may be possible in 3 to 6 months after completing physical therapy.
-
What kind of rehabilitation or physical therapy will I need post-surgery? A rehabilitation program focusing on strengthening the muscles around the spine, improving flexibility, and promoting healthy posture will be recommended.
7. What Should I Expect in Terms of Pain After Surgery?
-
How much pain or discomfort should I expect after the surgery? Mild to moderate pain is common in the initial post-operative period, but this should improve within a few weeks. The pain should be manageable with prescribed medications.
-
What pain management options are available, and for how long will I need them? Pain management may include prescription painkillers in the early stages, followed by over-the-counter medications like ibuprofen. Most patients can stop using pain medications after a few weeks.
-
Are there alternative methods to manage pain (e.g., ice packs, medications, relaxation techniques)? Ice packs, physical therapy, and relaxation techniques such as deep breathing or meditation can also help manage pain.
8. What Are the Costs and Insurance Coverage?
-
What is the total cost of the surgery, including pre-operative tests, the surgery itself, and post-operative care? The total cost can range between [insert cost range] depending on the hospital, location, and specific procedure.
-
Does my insurance cover the procedure, and if not, what are my financing options? Most insurance plans cover the procedure, but it’s best to confirm with your provider. Financing options may be available if needed.
-
Are there any hidden costs or additional charges I should be aware of? Be sure to ask about the cost of pre-operative tests, medications, and physical therapy that may not be covered by insurance.
9. What Happens If Surgery Does Not Work?
- What if the surgery does not relieve my symptoms or if the problem recurs? In rare cases, further surgery or alternative treatments may be required. We can explore options like additional spinal procedures or therapies.
10. What Are the Pre-Operative Instructions?
-
What do I need to do before surgery to prepare (e.g., fasting, medications to stop, or supplements to avoid)? Typically, you will need to fast for at least 6 hours before surgery and avoid certain medications like blood thinners or anti-inflammatory drugs.
-
Do I need to stop any medications or supplements before surgery, and how will that affect my health? Some medications, such as blood thinners, may need to be paused. Consult with your doctor about the medications you are currently taking.
-
Are there any lifestyle changes (e.g., stopping smoking or weight management) I should make before surgery to improve my outcomes? Smoking cessation and maintaining a healthy weight can significantly improve recovery outcomes.
11. Who Will Perform the Surgery, and How Experienced Are They?
-
Will the same surgeon who is consulting with me perform the surgery? Yes, I will be performing your surgery personally, and I have extensive experience with this procedure.
-
How many of these surgeries have you performed, and what is your success rate? I have performed [insert number] surgeries with a success rate of [insert success rate].
-
Will a surgical team assist, and what is their level of expertise? Yes, a skilled surgical team will assist, and each member has expertise in spinal surgeries.
12. Post-Operative Care and Follow-Up:
-
What post-operative care will I need, and how frequently will I need to follow up with you? Follow-up visits will be scheduled for the first few months to monitor healing and discuss physical therapy.
-
What kind of support or guidance will be available if I have concerns after surgery? A dedicated support team will be available for any questions or concerns, and I will be available for emergency consultation if necessary.
This comprehensive list of questions and answers will help you get the information you need before making an informed decision about your surgery.