Duration of Treatment
5 yo 6 hours Surgery
Days of Stay
5 to & days
Anesthesia
General Anesthesia
Cost
25000 to 35000 USD
How Much Does Epidural Stimulation Surgery Cost in India?
Looking for Epidural stimulation surgery Cost in India or a Top 10 Neurosurgeon at an affordable cost in different cities like Delhi, Mumbai, Chennai, Kolkata, and Bangalore? Here, we answer the question and explain how to choose the top 10 brain tumor treatment centers in India for better results.
We have also shortlisted the list of top Neuro treatment centers in India and Surgeons on the basis of Hospital accreditations, experience & qualification of surgeons, success rates of procedures, and patient testimonials.
- Epidural Stimulation Surgery Cost in India: Starting from 25,000 to 35,000 USD
- Hotel Cost Near Hospital - starting from 18 to 50 USD ( as per hotel services)
- Food Cost - starting from 20 to 30 USD (per day )
- Miscellaneous cost - 20 USD (per day)
It's only a rough estimate, final treatment will be planned after the fresh evaluation reports. Epidural Stimulation Surgery Cost in India can vary depending on the diagnosis, patient's conditions, surgeon experience, implant quality, hospital facilities, and city. To make an appointment, learn more about it, read the below information, or call / WhatsApp/ Viber - our experts to answer at +91 9582708782. Still, have questions?
What Is Epidural Stimulation Spinal Cord Injury Surgery?
Epidural stimulation spinal cord injury surgery is a revolutionary medical procedure designed to help individuals with spinal cord injuries regain motor function and control over their limbs. This technique involves implanting a device that delivers electrical currents to specific areas of the spinal cord, stimulating the neural pathways and enabling movements even in paralyzed individuals.
How It Works
The system consists of three main components:
- Electrode Array: Implanted on the spinal cord to deliver electrical stimulation.
- Pulse Generator: A small, battery-powered device implanted in the abdomen or hip area, connected to the electrodes.
- Remote Control Device: Used by patients and healthcare providers to adjust the intensity and pattern of stimulation.
Benefits of Epidural Stimulation Surgery
- Restoration of Movement: Many patients achieve significant improvements in voluntary control over their limbs.
- Improved Autonomic Functions: Enhanced bladder, bowel, and sexual functions are frequently reported.
- Enhanced Quality of Life: Patients regain independence in daily activities and reduce reliance on caregivers.
- Minimally Invasive: The surgery is less invasive compared to traditional spinal surgeries.
Who Can Benefit?
The surgery is suitable for individuals with:
- Chronic spinal cord injuries (complete or incomplete).
- Stable neurological condition post-injury.
- Strong commitment to post-surgical rehabilitation.
Who Is the Patient for Epidural Stimulation Spinal Cord Injury Surgery?
Epidural stimulation spinal cord injury surgery is a transformative treatment for individuals with spinal cord injuries (SCI). However, not all patients are candidates for this advanced procedure. Below is a detailed overview of the ideal patient profile for this surgery.
1. Types of Spinal Cord Injuries
Epidural stimulation surgery is primarily intended for patients with the following types of spinal cord injuries:
-
Complete Spinal Cord Injury (SCI):
Patients with complete SCI experience total loss of motor and sensory function below the injury level. Epidural stimulation can help activate dormant neural pathways to restore some voluntary movement. -
Incomplete Spinal Cord Injury (SCI):
Those with partial loss of function below the injury level often respond better to epidural stimulation because some neural pathways may still be intact.
2. Chronic Spinal Cord Injury
- Patients with stable, long-term injuries (at least 6-12 months post-injury) are considered ideal candidates. This is because the injury's severity and stability can be assessed more accurately during the chronic phase.
3. Level of Injury
-
Thoracic or Lumbar Injuries:
Most candidates for epidural stimulation have injuries in the thoracic or lumbar regions. This is because the surgery targets areas that control lower limb movements and autonomic functions. -
Cervical Injuries:
While rare, some patients with cervical injuries (affecting the neck region) may also benefit, particularly in improving autonomic functions like respiration, bladder, and bowel control.
4. Physical Condition of the Patient
-
Age:
Candidates can range from adolescents to older adults, but overall health and fitness play a role in determining eligibility. -
Body Mass Index (BMI):
A healthy BMI is preferred, as excessive body fat can interfere with device implantation. -
No Severe Comorbidities:
Patients with uncontrolled diabetes, severe infections, or other life-threatening conditions may not qualify.
5. Willingness to Commit to Rehabilitation
Epidural stimulation is not a standalone solution—it requires extensive post-surgery rehabilitation. Suitable candidates are those who:
- Are committed to working with physical therapists.
- Have the patience and motivation to engage in months of intensive training to regain movement.
6. Functional Goals of the Patient
The surgery is tailored to patients who aim to improve specific functions, such as:
- Motor Recovery: Regaining voluntary control over paralyzed limbs.
- Autonomic Functions: Enhancing bladder, bowel, and sexual function.
- Quality of Life: Achieving greater independence in daily activities.
7. Psychological Readiness
- Patients need to have realistic expectations about the surgery’s outcomes. While it can significantly improve functionality, it may not restore full mobility or sensation.
- Emotional stability and a strong support system are crucial for managing the challenges of rehabilitation.
8. Patients Who Have Tried Other Treatments
Epidural stimulation surgery is often recommended for patients who:
- Have not achieved satisfactory results with traditional therapies like physical therapy or medications.
- Are seeking innovative solutions after exhausting other treatment options.
Who May Not Be Suitable for Epidural Stimulation Surgery?
The following individuals may not be eligible for the procedure:
- Those with acute spinal cord injuries (less than 6 months post-injury).
- Patients with progressive neurological disorders like multiple sclerosis or ALS.
- Individuals with severe mental health disorders or substance abuse issues.
- Those unwilling or unable to commit to rehabilitation programs.
What will be The Risk Factors for Epidural Stimulation Spinal Cord Injury Surgery?
Epidural stimulation spinal cord injury surgery is a relatively safe and minimally invasive procedure. However, like any surgical intervention, it carries certain risks and potential complications. Understanding these risks helps patients make informed decisions and prepare adequately for the procedure.
Below are the main risk factors associated with this surgery:
1. Surgical Risks
a. Infection
- Risk: Infections can occur at the incision site or around the implanted device.
- Prevention: Proper surgical hygiene, postoperative wound care, and antibiotics reduce the risk.
- Management: Infections may require antibiotics or, in severe cases, removal of the device.
b. Bleeding or Hematoma
- Risk: Excessive bleeding or blood pooling (hematoma) near the surgical site.
- Prevention: Careful surgical technique and screening for blood clotting disorders.
c. Nerve Damage
- Risk: Accidental damage to nearby nerves during electrode placement, leading to pain, weakness, or sensory changes.
- Management: Most nerve-related issues are temporary, but severe cases may require further medical intervention.
d. Anesthesia Reactions
- Risk: Rare allergic reactions or complications related to anesthesia, including breathing difficulties or nausea.
- Prevention: Preoperative evaluation by an anesthesiologist to assess any risks.
2. Device-Related Risks
a. Lead Migration or Displacement
- Risk: The implanted leads (electrodes) may shift from their original position, reducing stimulation effectiveness.
- Management: Lead re-adjustment or repositioning surgery may be required.
b. Device Malfunction
- Risk: Faulty hardware, such as the pulse generator or electrodes, can affect stimulation delivery.
- Management: Repairs or replacement of the device may be necessary.
c. Battery Issues
- Risk: Battery depletion requiring replacement or malfunction of the pulse generator.
- Management: Regular follow-ups to monitor battery life and replace it when needed.
3. Neurological Risks
a. Increased Pain or Discomfort
- Risk: Some patients may experience new or increased pain due to nerve stimulation or device placement.
- Management: Adjusting stimulation settings or additional pain management strategies.
b. Temporary Worsening of Symptoms
- Risk: In rare cases, there may be a temporary increase in muscle spasms or other symptoms post-surgery.
- Management: These effects typically resolve with time or adjustments to the stimulation device.
c. Lack of Improvement
- Risk: Some patients may not experience significant improvements in motor or autonomic functions.
- Management: Comprehensive preoperative assessments help identify suitable candidates to minimize this risk.
4. General Postoperative Risks
a. Blood Clots (Deep Vein Thrombosis or Pulmonary Embolism)
- Risk: Reduced mobility after surgery can increase the risk of blood clots.
- Prevention: Early mobilization, compression stockings, and blood-thinning medications as prescribed.
b. Allergic Reactions
- Risk: Some patients may experience allergic reactions to the implanted device materials.
- Management: Preoperative testing and ensuring biocompatible materials are used.
c. Delayed Healing
- Risk: Factors such as diabetes, smoking, or poor nutrition may slow wound healing.
- Management: Optimizing health before surgery can reduce this risk.
5. Psychological Risks
a. Unrealistic Expectations
- Risk: Patients expecting complete recovery may feel disappointed if improvements are limited or gradual.
- Management: Preoperative counseling to set realistic goals and expectations.
b. Emotional Stress
- Risk: Dealing with postoperative recovery, adjustments to the device, and rehabilitation may cause emotional strain.
- Management: Support from psychologists, counselors, or support groups.
6. Risks Related to Comorbidities
Patients with underlying health conditions may face additional risks, such as:
- Cardiovascular Issues: Increased risk during anesthesia or surgery.
- Infections: Higher susceptibility for patients with diabetes or compromised immune systems.
Mitigating Risk Factors
-
Comprehensive Preoperative Evaluation
- Thorough medical history review, imaging, and physical exams to identify and address potential risks.
-
Choosing an Experienced Surgical Team
- Expertise in epidural stimulation surgery reduces the likelihood of complications.
-
Strict Adherence to Postoperative Care
- Following wound care instructions, avoiding strenuous activities, and attending all follow-up appointments.
-
Commitment to Rehabilitation
- A structured rehabilitation program helps optimize outcomes and minimize complications.
-
Lifestyle Modifications
- Quitting smoking, managing weight, and improving overall health before surgery reduce risks.
Success vs. Risk
While epidural stimulation surgery has certain risks, the potential benefits—such as regaining motor control, improving bowel and bladder function, and enhancing overall quality of life—often outweigh these concerns for suitable candidates. Each patient’s case is unique, and risks are minimized through careful planning, advanced surgical techniques, and comprehensive postoperative care.
Consulting with a specialized medical team ensures that the procedure is tailored to the individual, maximizing safety and effectiveness.
What will be the Preparation Before Epidural Stimulation Spinal Cord Injury Surgery?
Proper preparation is crucial for the success of epidural stimulation spinal cord injury surgery. This includes medical assessments, mental readiness, and practical planning to ensure the procedure and post-operative rehabilitation proceed smoothly. Below is a step-by-step guide to the preparation process:
1. Comprehensive Medical Evaluation
Before undergoing epidural stimulation surgery, patients must undergo a detailed medical assessment to determine their suitability for the procedure.
a. Medical History Review
- Analysis of the patient’s spinal cord injury details, including the type (complete or incomplete), level of injury, and time since the injury.
- Review of any previous treatments or surgeries related to the spinal cord injury.
- Identification of underlying medical conditions such as diabetes, infections, or cardiovascular issues that could affect surgery or recovery.
b. Diagnostic Tests
- MRI or CT Scans: To assess the structure and condition of the spinal cord and surrounding tissues.
- X-rays: To evaluate spinal alignment and detect any complications.
- Electromyography (EMG): To measure electrical activity in muscles and assess the potential for nerve stimulation.
c. Neurological Assessment
A detailed evaluation of the patient's motor and sensory functions to establish a baseline for comparison post-surgery.
2. Psychological Assessment
Preparing mentally and emotionally for the procedure is equally important. The surgery requires commitment to rehabilitation and a positive outlook toward recovery.
- Counseling Sessions: To set realistic expectations about the outcomes of the surgery.
- Support System: Involvement of family or caregivers who can assist the patient during recovery and rehabilitation.
3. Physical Conditioning
Improving physical health before surgery can enhance recovery and maximize the benefits of the procedure.
a. Nutritional Support
- Following a balanced diet to boost immunity and promote healing.
- Ensuring adequate protein intake to support tissue repair and muscle strength.
b. Physical Therapy
- Engaging in pre-surgery exercises to maintain flexibility and strength in the unaffected parts of the body.
- Strengthening core muscles to support overall stability.
c. Weight Management
- Maintaining a healthy weight to reduce surgical risks and improve device implantation outcomes.
4. Pre-Surgical Tests
Certain standard tests are performed to ensure the patient is fit for anesthesia and surgery:
- Blood Tests: To check for anemia, infections, or any clotting issues.
- Urinalysis: To detect any urinary infections.
- Cardiovascular Tests: Such as ECG or stress tests, especially for older patients or those with heart conditions.
5. Trial Stimulation
Before permanent implantation, most patients undergo a trial stimulation phase to evaluate the potential effectiveness of epidural stimulation.
- Temporary Electrode Placement: A small electrode is implanted temporarily to test the patient’s response to electrical stimulation.
- Assessment Period: Over several days, healthcare providers monitor improvements in motor functions or autonomic responses (e.g., bladder or bowel control).
- Decision Making: If the trial is successful, the patient proceeds with permanent implantation.
6. Medication Adjustments
Patients may need to modify their current medications before surgery:
- Stop Certain Medications: Such as blood thinners, to minimize bleeding risks.
- Pain Management: Adjustments to existing pain medications to avoid interactions with anesthesia.
- Infection Control: Antibiotics may be prescribed to prevent infections.
7. Lifestyle Changes
Adopting specific lifestyle changes can optimize surgical outcomes:
- Quit Smoking: Smoking can impair wound healing and increase the risk of complications.
- Limit Alcohol: Reducing alcohol intake helps maintain overall health and ensures medications work effectively.
- Manage Stress: Practicing relaxation techniques like meditation or breathing exercises can reduce pre-surgery anxiety.
8. Practical Arrangements
a. Hospital Stay
- Prepare for a short hospital stay for the procedure and initial monitoring.
b. Transportation
- Arrange for transportation to and from the hospital.
c. Post-Surgery Care
- Set up a comfortable recovery space at home with easy access to essentials.
- Arrange for a caregiver to assist with daily tasks during the initial recovery period.
9. Pre-Surgical Instructions
Patients will receive specific instructions from their surgeon, such as:
- Fasting Requirements: Avoid food or drinks for a set period before surgery.
- Hygiene Protocols: Cleaning the surgical site with antiseptic solutions.
- Clothing: Wear loose-fitting clothes on the day of surgery.
10. Address Questions and Concerns
Before the procedure, patients should discuss any concerns or questions with their healthcare team, such as:
- What to expect during the surgery.
- Potential risks and benefits.
- Details of the post-operative rehabilitation program
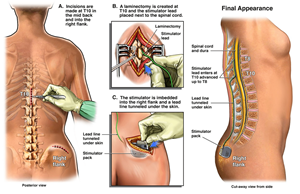
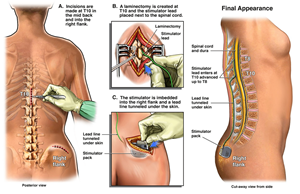
Procedure for Epidural Stimulation Spinal Cord Injury Surgery
Epidural stimulation surgery for spinal cord injury is a groundbreaking technique aimed at restoring lost motor functions, improving autonomic functions, and enhancing the quality of life for individuals with spinal cord injuries. The procedure involves implanting a device that delivers electrical stimulation to the spinal cord, bypassing damaged pathways and activating dormant neural circuits. Below is a detailed breakdown of the surgical process.
1. Preoperative Phase
a. Anesthesia
- The patient is administered general or local anesthesia to ensure comfort during the procedure.
b. Positioning
- The patient is positioned on the operating table, typically lying face down, to provide access to the lower back area.
c. Sterilization
- The surgical site is cleaned and sterilized to minimize the risk of infection.
2. Surgical Steps
Step 1: Incision
- A small incision is made in the lower back to expose the vertebrae near the spinal cord where the electrodes will be placed.
Step 2: Electrode Placement
- Electrodes: Thin, flexible electrodes are carefully inserted into the epidural space (the area surrounding the spinal cord).
- Targeted Areas: The electrodes are positioned over specific spinal segments responsible for motor and autonomic functions.
Step 3: Connection to Pulse Generator
- A lead wire from the electrodes is tunneled under the skin and connected to a pulse generator.
- The pulse generator, a small device that controls the electrical impulses, is implanted under the skin, typically in the abdomen or buttocks.
Step 4: Testing and Adjustment
- During the surgery, the electrodes are tested to ensure correct placement and functionality.
- The surgeon and a neurologist may work together to confirm that the stimulation activates the desired spinal cord regions.
3. Post-Placement Programming
a. Initial Programming
- After the device is implanted, it is programmed using an external controller.
- The settings are customized to the patient’s specific needs, targeting motor control, bladder and bowel regulation, or other autonomic functions.
b. Calibration
- The stimulation intensity, frequency, and patterns are adjusted over several sessions post-surgery to achieve optimal results.
4. Closing the Incisions
a. Securing the Device
- The electrodes and pulse generator are secured in place to prevent movement.
b. Suturing
- The incisions are closed using sutures or surgical staples and covered with sterile dressings.
5. Postoperative Monitoring
a. Recovery Room
- The patient is moved to a recovery room for close monitoring of vital signs and surgical site.
b. Initial Testing
- The stimulation device is tested again post-surgery to confirm proper functioning.
c. Pain Management
- Pain medications may be administered to manage post-surgical discomfort.
6. Follow-Up and Rehabilitation
a. Regular Follow-Ups
- Follow-up appointments are scheduled to monitor the patient’s recovery and adjust device settings as needed.
b. Physical Therapy
- Patients participate in a customized rehabilitation program to maximize the benefits of the epidural stimulation.
- Therapy focuses on relearning movements and improving strength and coordination.
c. Device Management
- Patients are trained on how to use the external controller to adjust settings and manage stimulation sessions.
Key Goals of the Procedure
- Restoration of Motor Functions
- Activate dormant neural circuits to facilitate voluntary movements.
- Improvement in Autonomic Functions
- Enhance bladder and bowel control, sexual function, and cardiovascular stability.
- Reduction in Secondary Complications
- Improve circulation, reduce pressure sores, and prevent muscle atrophy.
Duration of the Surgery
The entire procedure typically takes 2 to 4 hours, depending on the complexity of the case and the number of electrodes being implanted.
Risks and Complications
Although the surgery is generally safe, potential risks include:
- Infection at the surgical site.
- Electrode displacement or malfunction.
- Pain or discomfort near the pulse generator.
- Skin irritation over the implanted device.
Conclusion
Epidural stimulation spinal cord injury surgery is a sophisticated and innovative procedure that requires precision and expertise. By directly targeting the spinal cord with electrical stimulation, this technique offers hope to individuals with spinal cord injuries, enabling them to regain motor and autonomic functions that were previously thought to be permanently lost.
What will be the postcare of Epidural Stimulation Spinal Cord Injury Surgery patient?
Post care for Epidural Stimulation Spinal Cord Injury Surgery Patients
Postoperative care is a critical phase in the recovery process following epidural stimulation spinal cord injury surgery. It involves medical supervision, lifestyle adjustments, and rehabilitation to ensure optimal healing, proper functioning of the implanted device, and the best possible outcomes for regaining motor and autonomic functions.
1. Immediate Postoperative Care
a. Hospital Stay
- Duration: Patients typically stay in the hospital for 2–5 days for initial monitoring.
- Vital Signs Monitoring: Blood pressure, heart rate, and other vital signs are closely observed.
- Pain Management: Medications such as analgesics are administered to manage surgical discomfort.
b. Wound Care
- Surgical sites (incisions for electrodes and pulse generator) are checked daily for signs of infection or bleeding.
- Dressings are changed as per the surgeon's instructions.
c. Device Function Testing
- The implanted device is tested to ensure proper electrode placement and functioning.
- Adjustments may be made to initial stimulation settings.
2. Discharge Instructions
a. Medication Management
- Painkillers and antibiotics are prescribed to prevent discomfort and infections.
- Patients should follow a strict medication schedule.
b. Physical Activity Restrictions
- Avoid strenuous activities, heavy lifting, or twisting motions for 4–6 weeks to allow proper healing of the surgical site.
- Gradual mobility improvements are encouraged with the guidance of a healthcare provider.
c. Incision Care
- Keep the surgical sites clean and dry.
- Avoid soaking in baths or swimming pools until the incisions are fully healed.
- Watch for signs of infection, such as redness, swelling, or discharge, and report them to the doctor immediately.
3. Follow-Up Appointments
a. Wound Check
- Scheduled 1–2 weeks after surgery to assess incision healing.
- Sutures or staples, if present, are removed during this visit.
b. Device Programming
- The device settings are fine-tuned in follow-up appointments based on patient feedback and responses.
- Adjustments are aimed at optimizing stimulation for desired motor or autonomic improvements.
4. Rehabilitation Therapy
Rehabilitation plays a vital role in enhancing the outcomes of epidural stimulation surgery. A multidisciplinary team, including physical therapists, occupational therapists, and neurologists, supports the recovery process.
a. Physical Therapy
- Focuses on regaining strength, flexibility, and coordination.
- Exercises are designed to improve voluntary movements in areas affected by the spinal cord injury.
b. Gait Training
- If the patient shows progress in lower limb movements, walking exercises with assistive devices may be introduced.
- Therapists provide guidance on safe mobility techniques.
c. Autonomic Function Training
- Patients may undergo training to improve bowel and bladder control, manage blood pressure, and enhance sexual functions.
5. Long-Term Device Management
a. Using the External Controller
- Patients are taught how to operate the external controller to adjust stimulation levels as needed.
- Training includes turning the device on and off and understanding how to respond to changes in stimulation effects.
b. Regular Maintenance
- Periodic check-ups are scheduled to assess the device’s functionality and battery life.
- Battery replacement for the pulse generator may be required every 5–10 years, depending on usage.
c. Troubleshooting
- Patients are advised to report any unusual sensations, reduced stimulation effectiveness, or discomfort near the device to their healthcare provider.
6. Lifestyle Adjustments
a. Diet and Nutrition
- A balanced diet is recommended to support overall healing and recovery.
- High-fiber foods and adequate hydration help maintain bowel health, especially if autonomic functions are affected.
b. Hygiene and Skin Care
- Prevent pressure sores by changing positions frequently and using supportive cushions or mattresses.
- Maintain good hygiene, especially around the surgical sites.
c. Stress Management
- Psychological counseling or support groups can help patients cope with the emotional challenges of recovery.
7. Signs of Complications to Watch For
Patients should contact their healthcare provider immediately if they notice:
- Persistent or worsening pain at the surgical site.
- Signs of infection: fever, redness, swelling, or discharge.
- Malfunction of the implanted device, such as loss of stimulation or irregular sensations.
- Difficulty in movement or worsening symptoms.
8. Long-Term Outcomes
a. Functional Improvements
- With consistent rehabilitation and device optimization, many patients experience improvements in motor function, autonomic regulation, and quality of life.
b. Gradual Progress
- Recovery and functional gains may occur gradually over weeks or months as the body adapts to the device and rehabilitation exercises.
c. Lifelong Commitment
- Commitment to follow-up appointments, rehabilitation, and device management is essential for sustained benefits.
What will be the success rate of Epidural Stimulation Spinal Cord Injury Surgery?
The success rate of epidural stimulation spinal cord injury (SCI) surgery depends on various factors, including the type and severity of the spinal cord injury, the patient's overall health, adherence to post-surgery rehabilitation, and the goals of the treatment. While exact success rates can vary, clinical studies and patient outcomes have demonstrated significant improvements in motor and autonomic functions for many individuals undergoing this procedure.
Key Metrics of Success
1. Motor Function Improvement
- Success Rate: Approximately 60–80% of patients experience meaningful improvements in voluntary movements, particularly in the lower limbs.
- Details:
- Patients with incomplete spinal cord injuries often show greater recovery potential than those with complete injuries.
- Movements may include the ability to flex knees, wiggle toes, or lift legs under controlled conditions.
2. Autonomic Function Restoration
- Success Rate: Up to 70% of patients report improved bladder, bowel, and sexual function.
- Details:
- Enhanced bladder control reduces dependence on catheters.
- Improved bowel control allows for a more regular and independent bowel routine.
- Many patients also experience better regulation of blood pressure and reduced orthostatic hypotension.
3. Reduction in Secondary Complications
- Improved Quality of Life: A high proportion of patients report fewer complications such as pressure sores, muscle atrophy, and poor circulation.
- Success Rate: About 80–90% of patients see improvements in circulation and muscle health with regular use of the stimulation device.
4. Overall Patient Satisfaction
- Satisfaction Rate: Around 85% of patients express satisfaction with the procedure, citing improved independence, mobility, and quality of life.
- Details:
- Psychological benefits, such as reduced anxiety and depression, are often reported due to regained functional abilities.
Factors Influencing Success
-
Type of Injury
- Incomplete Injuries: Higher success rates, as some neural pathways remain intact.
- Complete Injuries: Progress is slower and may require more extensive rehabilitation.
-
Time Since Injury
- Early intervention generally leads to better outcomes, but even patients with long-term injuries have shown improvements.
-
Rehabilitation Commitment
- Patients who actively participate in post-surgery physical therapy and rehabilitation programs tend to achieve better results.
-
Device Programming and Adjustments
- Customization of the stimulation settings to meet individual needs significantly enhances the efficacy of the procedure.
-
Health and Age
- Younger patients and those without additional health complications often experience faster recovery and better results.
Challenges and Limitations
-
Complete Restoration of Function
- While many patients regain some degree of motor or autonomic function, complete recovery is rare, particularly in cases of severe or complete spinal cord injuries.
-
Time for Visible Results
- Functional improvements may take weeks or months of consistent therapy and device adjustments to become evident.
-
Variability in Response
- Not all patients respond equally; some may achieve only minimal improvements.
Clinical Evidence
Several studies and clinical trials have documented the success rates and outcomes of epidural stimulation:
-
Motor Function Recovery
- A study published in Nature Medicine found that 80% of patients with incomplete SCI achieved significant voluntary movement with epidural stimulation and intensive rehabilitation.
-
Autonomic Improvements
- Research by the Christopher & Dana Reeve Foundation reported that 70% of participants experienced improved bladder and bowel control, alongside better blood pressure regulation.
-
Long-Term Benefits
- Follow-up studies have shown that many patients retain their improvements for years, provided they maintain regular use of the stimulation device and follow their rehabilitation plan.
FAQ: Epidural Stimulation Spinal Cord Injury Surgery
Epidural stimulation surgery for spinal cord injuries has gained attention for its ability to improve motor and autonomic functions in patients with spinal cord injuries (SCI). Below are some frequently asked questions (FAQs) about the procedure, its benefits, and its cost in India.
1. What is Epidural Stimulation Spinal Cord Injury Surgery?
Answer:
Epidural stimulation involves the implantation of a device that delivers electrical impulses to the lower spinal cord. These impulses help activate neural circuits responsible for movement and autonomic functions, potentially restoring partial voluntary control in individuals with spinal cord injuries.
2. Who is a Candidate for Epidural Stimulation Surgery?
Answer:
This surgery is suitable for individuals with:
- Chronic spinal cord injuries (both complete and incomplete).
- Minimal or no response to conventional therapies.
- A stable health condition to undergo surgery and rehabilitation.
A thorough evaluation by a medical team is necessary to determine eligibility.
3. What Benefits Can Patients Expect?
Answer:
- Improved voluntary motor control in lower limbs.
- Enhanced bladder and bowel function.
- Better blood pressure regulation.
- Increased independence in daily activities.
- Improved quality of life through regained partial mobility.
4. What is the Procedure for Epidural Stimulation Surgery?
Answer:
The procedure involves:
- Preoperative Assessment: Medical tests and evaluations to determine suitability.
- Device Implantation: Electrodes are implanted on the spinal cord, and a pulse generator is placed under the skin.
- Device Programming: The stimulation device is adjusted to the patient’s specific needs.
- Rehabilitation: Post-surgery physical therapy to maximize benefits.
5. What are the Risks and Complications?
Answer:
- Infection at the surgical site.
- Displacement of electrodes or malfunction of the device.
- Temporary pain or discomfort.
- Lack of improvement in some cases.
- Rarely, nerve damage.
These risks are minimized through proper preoperative evaluation, skilled surgical techniques, and postoperative care.
6. How Long Does Recovery Take?
Answer:
Recovery varies by individual, but typically:
- Initial recovery from surgery: 1–2 weeks.
- Rehabilitation and therapy: Ongoing for several months to achieve optimal results.
Patients must adhere to follow-up appointments and rehabilitation programs.
7. Why Choose India for Epidural Stimulation Surgery?
Answer:
India is a preferred destination for this procedure due to:
- Highly skilled surgeons specializing in spinal cord injury treatments.
- Advanced medical facilities with state-of-the-art technology.
- Affordable costs compared to Western countries.
- Comprehensive rehabilitation services.
8. How Much Does Epidural Stimulation Surgery Cost in India?
Answer:
The epidural stimulation surgery cost in India typically ranges from ₹20,00,000 to ₹35,00,000 (approximately USD 25,000 to USD 35,000).
This includes:
- Preoperative evaluation.
- Surgery and hospitalization.
- Cost of the implant (stimulation device).
- Postoperative follow-up and initial rehabilitation.
9. Does Health Insurance Cover Epidural Stimulation Surgery?
Answer:
Coverage depends on the insurance provider and the patient’s policy. Some international insurance plans may cover the procedure if it is medically indicated. Patients are advised to check with their insurance providers for specific coverage details.
10. Which Hospitals in India Offer Epidural Stimulation Surgery?
Answer:
Some of the leading hospitals providing this surgery include:
- IBS Hospital, New Delhi
- Amrita Hospital, New Delhi
- Apollo Hospitals, Chennai/Delhi/Mumbai
- Fortis Hospitals, Bangalore/Gurgaon
- Manipal Hospitals, Bangalore
- Medanta – The Medicity, Gurgaon
- Max Super Specialty Hospital, Delhi
- Kokilaben Dhirubhai Ambani Hospital, Mumbai
11. What Are the Success Rates of the Procedure?
Answer:
- Approximately 60–80% of patients experience significant improvement in motor function.
- Up to 70% report enhanced bladder, bowel, and blood pressure control.
- Success depends on factors like the severity of injury, patient health, and rehabilitation commitment.
12. What Kind of Postoperative Care is Required?
Answer:
- Regular follow-ups to monitor device function and adjust settings.
- Adherence to a customized rehabilitation program.
- Maintaining proper wound care and avoiding strenuous activities during initial recovery.
13. Is the Surgery Permanent?
Answer:
The implanted device is designed to be long-lasting, but the pulse generator may require replacement every 5–10 years, depending on the battery life and usage.
14. How Can I Prepare for the Surgery?
Answer:
Preparation includes:
- Medical evaluations and tests.
- Stopping certain medications as advised.
- Lifestyle changes like quitting smoking and improving overall fitness.
15. How Can I Get Started with Epidural Stimulation Surgery in India?
Answer:
- Consult a Specialist: Contact a hospital with expertise in spinal cord injury treatments.
- Medical Assessment: Provide your medical records for an evaluation.
- Travel Arrangements: Plan your visit with the hospital’s international patient care team if you’re traveling from abroad.
- Plan for Rehabilitation: Set aside time for postoperative therapy in India or your home country.
Top Doctors
Sorry, There is nothing to show!Come back soon.
Top Hospitals
Epidural Stimulation Spinal Cord Surgery Cost in India
Duration of Treatment
5 yo 6 hours Surgery
Days of Stay
5 to & days
Anesthesia
General Anesthesia
Cost
25000 to 35000 USD
How Much Does Epidural Stimulation Surgery Cost in India?
Looking for Epidural stimulation surgery Cost in India or a Top 10 Neurosurgeon at an affordable cost in different cities like Delhi, Mumbai, Chennai, Kolkata, and Bangalore? Here, we answer the question and explain how to choose the top 10 brain tumor treatment centers in India for better results.
We have also shortlisted the list of top Neuro treatment centers in India and Surgeons on the basis of Hospital accreditations, experience & qualification of surgeons, success rates of procedures, and patient testimonials.
- Epidural Stimulation Surgery Cost in India: Starting from 25,000 to 35,000 USD
- Hotel Cost Near Hospital - starting from 18 to 50 USD ( as per hotel services)
- Food Cost - starting from 20 to 30 USD (per day )
- Miscellaneous cost - 20 USD (per day)
It's only a rough estimate, final treatment will be planned after the fresh evaluation reports. Epidural Stimulation Surgery Cost in India can vary depending on the diagnosis, patient's conditions, surgeon experience, implant quality, hospital facilities, and city. To make an appointment, learn more about it, read the below information, or call / WhatsApp/ Viber - our experts to answer at +91 9582708782. Still, have questions?
What Is Epidural Stimulation Spinal Cord Injury Surgery?
Epidural stimulation spinal cord injury surgery is a revolutionary medical procedure designed to help individuals with spinal cord injuries regain motor function and control over their limbs. This technique involves implanting a device that delivers electrical currents to specific areas of the spinal cord, stimulating the neural pathways and enabling movements even in paralyzed individuals.
How It Works
The system consists of three main components:
- Electrode Array: Implanted on the spinal cord to deliver electrical stimulation.
- Pulse Generator: A small, battery-powered device implanted in the abdomen or hip area, connected to the electrodes.
- Remote Control Device: Used by patients and healthcare providers to adjust the intensity and pattern of stimulation.
Benefits of Epidural Stimulation Surgery
- Restoration of Movement: Many patients achieve significant improvements in voluntary control over their limbs.
- Improved Autonomic Functions: Enhanced bladder, bowel, and sexual functions are frequently reported.
- Enhanced Quality of Life: Patients regain independence in daily activities and reduce reliance on caregivers.
- Minimally Invasive: The surgery is less invasive compared to traditional spinal surgeries.
Who Can Benefit?
The surgery is suitable for individuals with:
- Chronic spinal cord injuries (complete or incomplete).
- Stable neurological condition post-injury.
- Strong commitment to post-surgical rehabilitation.
symptoms
Who Is the Patient for Epidural Stimulation Spinal Cord Injury Surgery?
Epidural stimulation spinal cord injury surgery is a transformative treatment for individuals with spinal cord injuries (SCI). However, not all patients are candidates for this advanced procedure. Below is a detailed overview of the ideal patient profile for this surgery.
1. Types of Spinal Cord Injuries
Epidural stimulation surgery is primarily intended for patients with the following types of spinal cord injuries:
-
Complete Spinal Cord Injury (SCI):
Patients with complete SCI experience total loss of motor and sensory function below the injury level. Epidural stimulation can help activate dormant neural pathways to restore some voluntary movement. -
Incomplete Spinal Cord Injury (SCI):
Those with partial loss of function below the injury level often respond better to epidural stimulation because some neural pathways may still be intact.
2. Chronic Spinal Cord Injury
- Patients with stable, long-term injuries (at least 6-12 months post-injury) are considered ideal candidates. This is because the injury's severity and stability can be assessed more accurately during the chronic phase.
3. Level of Injury
-
Thoracic or Lumbar Injuries:
Most candidates for epidural stimulation have injuries in the thoracic or lumbar regions. This is because the surgery targets areas that control lower limb movements and autonomic functions. -
Cervical Injuries:
While rare, some patients with cervical injuries (affecting the neck region) may also benefit, particularly in improving autonomic functions like respiration, bladder, and bowel control.
4. Physical Condition of the Patient
-
Age:
Candidates can range from adolescents to older adults, but overall health and fitness play a role in determining eligibility. -
Body Mass Index (BMI):
A healthy BMI is preferred, as excessive body fat can interfere with device implantation. -
No Severe Comorbidities:
Patients with uncontrolled diabetes, severe infections, or other life-threatening conditions may not qualify.
5. Willingness to Commit to Rehabilitation
Epidural stimulation is not a standalone solution—it requires extensive post-surgery rehabilitation. Suitable candidates are those who:
- Are committed to working with physical therapists.
- Have the patience and motivation to engage in months of intensive training to regain movement.
6. Functional Goals of the Patient
The surgery is tailored to patients who aim to improve specific functions, such as:
- Motor Recovery: Regaining voluntary control over paralyzed limbs.
- Autonomic Functions: Enhancing bladder, bowel, and sexual function.
- Quality of Life: Achieving greater independence in daily activities.
7. Psychological Readiness
- Patients need to have realistic expectations about the surgery’s outcomes. While it can significantly improve functionality, it may not restore full mobility or sensation.
- Emotional stability and a strong support system are crucial for managing the challenges of rehabilitation.
8. Patients Who Have Tried Other Treatments
Epidural stimulation surgery is often recommended for patients who:
- Have not achieved satisfactory results with traditional therapies like physical therapy or medications.
- Are seeking innovative solutions after exhausting other treatment options.
Who May Not Be Suitable for Epidural Stimulation Surgery?
The following individuals may not be eligible for the procedure:
- Those with acute spinal cord injuries (less than 6 months post-injury).
- Patients with progressive neurological disorders like multiple sclerosis or ALS.
- Individuals with severe mental health disorders or substance abuse issues.
- Those unwilling or unable to commit to rehabilitation programs.
risk factors
What will be The Risk Factors for Epidural Stimulation Spinal Cord Injury Surgery?
Epidural stimulation spinal cord injury surgery is a relatively safe and minimally invasive procedure. However, like any surgical intervention, it carries certain risks and potential complications. Understanding these risks helps patients make informed decisions and prepare adequately for the procedure.
Below are the main risk factors associated with this surgery:
1. Surgical Risks
a. Infection
- Risk: Infections can occur at the incision site or around the implanted device.
- Prevention: Proper surgical hygiene, postoperative wound care, and antibiotics reduce the risk.
- Management: Infections may require antibiotics or, in severe cases, removal of the device.
b. Bleeding or Hematoma
- Risk: Excessive bleeding or blood pooling (hematoma) near the surgical site.
- Prevention: Careful surgical technique and screening for blood clotting disorders.
c. Nerve Damage
- Risk: Accidental damage to nearby nerves during electrode placement, leading to pain, weakness, or sensory changes.
- Management: Most nerve-related issues are temporary, but severe cases may require further medical intervention.
d. Anesthesia Reactions
- Risk: Rare allergic reactions or complications related to anesthesia, including breathing difficulties or nausea.
- Prevention: Preoperative evaluation by an anesthesiologist to assess any risks.
2. Device-Related Risks
a. Lead Migration or Displacement
- Risk: The implanted leads (electrodes) may shift from their original position, reducing stimulation effectiveness.
- Management: Lead re-adjustment or repositioning surgery may be required.
b. Device Malfunction
- Risk: Faulty hardware, such as the pulse generator or electrodes, can affect stimulation delivery.
- Management: Repairs or replacement of the device may be necessary.
c. Battery Issues
- Risk: Battery depletion requiring replacement or malfunction of the pulse generator.
- Management: Regular follow-ups to monitor battery life and replace it when needed.
3. Neurological Risks
a. Increased Pain or Discomfort
- Risk: Some patients may experience new or increased pain due to nerve stimulation or device placement.
- Management: Adjusting stimulation settings or additional pain management strategies.
b. Temporary Worsening of Symptoms
- Risk: In rare cases, there may be a temporary increase in muscle spasms or other symptoms post-surgery.
- Management: These effects typically resolve with time or adjustments to the stimulation device.
c. Lack of Improvement
- Risk: Some patients may not experience significant improvements in motor or autonomic functions.
- Management: Comprehensive preoperative assessments help identify suitable candidates to minimize this risk.
4. General Postoperative Risks
a. Blood Clots (Deep Vein Thrombosis or Pulmonary Embolism)
- Risk: Reduced mobility after surgery can increase the risk of blood clots.
- Prevention: Early mobilization, compression stockings, and blood-thinning medications as prescribed.
b. Allergic Reactions
- Risk: Some patients may experience allergic reactions to the implanted device materials.
- Management: Preoperative testing and ensuring biocompatible materials are used.
c. Delayed Healing
- Risk: Factors such as diabetes, smoking, or poor nutrition may slow wound healing.
- Management: Optimizing health before surgery can reduce this risk.
5. Psychological Risks
a. Unrealistic Expectations
- Risk: Patients expecting complete recovery may feel disappointed if improvements are limited or gradual.
- Management: Preoperative counseling to set realistic goals and expectations.
b. Emotional Stress
- Risk: Dealing with postoperative recovery, adjustments to the device, and rehabilitation may cause emotional strain.
- Management: Support from psychologists, counselors, or support groups.
6. Risks Related to Comorbidities
Patients with underlying health conditions may face additional risks, such as:
- Cardiovascular Issues: Increased risk during anesthesia or surgery.
- Infections: Higher susceptibility for patients with diabetes or compromised immune systems.
Mitigating Risk Factors
-
Comprehensive Preoperative Evaluation
- Thorough medical history review, imaging, and physical exams to identify and address potential risks.
-
Choosing an Experienced Surgical Team
- Expertise in epidural stimulation surgery reduces the likelihood of complications.
-
Strict Adherence to Postoperative Care
- Following wound care instructions, avoiding strenuous activities, and attending all follow-up appointments.
-
Commitment to Rehabilitation
- A structured rehabilitation program helps optimize outcomes and minimize complications.
-
Lifestyle Modifications
- Quitting smoking, managing weight, and improving overall health before surgery reduce risks.
Success vs. Risk
While epidural stimulation surgery has certain risks, the potential benefits—such as regaining motor control, improving bowel and bladder function, and enhancing overall quality of life—often outweigh these concerns for suitable candidates. Each patient’s case is unique, and risks are minimized through careful planning, advanced surgical techniques, and comprehensive postoperative care.
Consulting with a specialized medical team ensures that the procedure is tailored to the individual, maximizing safety and effectiveness.
preparation
What will be the Preparation Before Epidural Stimulation Spinal Cord Injury Surgery?
Proper preparation is crucial for the success of epidural stimulation spinal cord injury surgery. This includes medical assessments, mental readiness, and practical planning to ensure the procedure and post-operative rehabilitation proceed smoothly. Below is a step-by-step guide to the preparation process:
1. Comprehensive Medical Evaluation
Before undergoing epidural stimulation surgery, patients must undergo a detailed medical assessment to determine their suitability for the procedure.
a. Medical History Review
- Analysis of the patient’s spinal cord injury details, including the type (complete or incomplete), level of injury, and time since the injury.
- Review of any previous treatments or surgeries related to the spinal cord injury.
- Identification of underlying medical conditions such as diabetes, infections, or cardiovascular issues that could affect surgery or recovery.
b. Diagnostic Tests
- MRI or CT Scans: To assess the structure and condition of the spinal cord and surrounding tissues.
- X-rays: To evaluate spinal alignment and detect any complications.
- Electromyography (EMG): To measure electrical activity in muscles and assess the potential for nerve stimulation.
c. Neurological Assessment
A detailed evaluation of the patient's motor and sensory functions to establish a baseline for comparison post-surgery.
2. Psychological Assessment
Preparing mentally and emotionally for the procedure is equally important. The surgery requires commitment to rehabilitation and a positive outlook toward recovery.
- Counseling Sessions: To set realistic expectations about the outcomes of the surgery.
- Support System: Involvement of family or caregivers who can assist the patient during recovery and rehabilitation.
3. Physical Conditioning
Improving physical health before surgery can enhance recovery and maximize the benefits of the procedure.
a. Nutritional Support
- Following a balanced diet to boost immunity and promote healing.
- Ensuring adequate protein intake to support tissue repair and muscle strength.
b. Physical Therapy
- Engaging in pre-surgery exercises to maintain flexibility and strength in the unaffected parts of the body.
- Strengthening core muscles to support overall stability.
c. Weight Management
- Maintaining a healthy weight to reduce surgical risks and improve device implantation outcomes.
4. Pre-Surgical Tests
Certain standard tests are performed to ensure the patient is fit for anesthesia and surgery:
- Blood Tests: To check for anemia, infections, or any clotting issues.
- Urinalysis: To detect any urinary infections.
- Cardiovascular Tests: Such as ECG or stress tests, especially for older patients or those with heart conditions.
5. Trial Stimulation
Before permanent implantation, most patients undergo a trial stimulation phase to evaluate the potential effectiveness of epidural stimulation.
- Temporary Electrode Placement: A small electrode is implanted temporarily to test the patient’s response to electrical stimulation.
- Assessment Period: Over several days, healthcare providers monitor improvements in motor functions or autonomic responses (e.g., bladder or bowel control).
- Decision Making: If the trial is successful, the patient proceeds with permanent implantation.
6. Medication Adjustments
Patients may need to modify their current medications before surgery:
- Stop Certain Medications: Such as blood thinners, to minimize bleeding risks.
- Pain Management: Adjustments to existing pain medications to avoid interactions with anesthesia.
- Infection Control: Antibiotics may be prescribed to prevent infections.
7. Lifestyle Changes
Adopting specific lifestyle changes can optimize surgical outcomes:
- Quit Smoking: Smoking can impair wound healing and increase the risk of complications.
- Limit Alcohol: Reducing alcohol intake helps maintain overall health and ensures medications work effectively.
- Manage Stress: Practicing relaxation techniques like meditation or breathing exercises can reduce pre-surgery anxiety.
8. Practical Arrangements
a. Hospital Stay
- Prepare for a short hospital stay for the procedure and initial monitoring.
b. Transportation
- Arrange for transportation to and from the hospital.
c. Post-Surgery Care
- Set up a comfortable recovery space at home with easy access to essentials.
- Arrange for a caregiver to assist with daily tasks during the initial recovery period.
9. Pre-Surgical Instructions
Patients will receive specific instructions from their surgeon, such as:
- Fasting Requirements: Avoid food or drinks for a set period before surgery.
- Hygiene Protocols: Cleaning the surgical site with antiseptic solutions.
- Clothing: Wear loose-fitting clothes on the day of surgery.
10. Address Questions and Concerns
Before the procedure, patients should discuss any concerns or questions with their healthcare team, such as:
- What to expect during the surgery.
- Potential risks and benefits.
- Details of the post-operative rehabilitation program
procedure
Procedure for Epidural Stimulation Spinal Cord Injury Surgery
Epidural stimulation surgery for spinal cord injury is a groundbreaking technique aimed at restoring lost motor functions, improving autonomic functions, and enhancing the quality of life for individuals with spinal cord injuries. The procedure involves implanting a device that delivers electrical stimulation to the spinal cord, bypassing damaged pathways and activating dormant neural circuits. Below is a detailed breakdown of the surgical process.
1. Preoperative Phase
a. Anesthesia
- The patient is administered general or local anesthesia to ensure comfort during the procedure.
b. Positioning
- The patient is positioned on the operating table, typically lying face down, to provide access to the lower back area.
c. Sterilization
- The surgical site is cleaned and sterilized to minimize the risk of infection.
2. Surgical Steps
Step 1: Incision
- A small incision is made in the lower back to expose the vertebrae near the spinal cord where the electrodes will be placed.
Step 2: Electrode Placement
- Electrodes: Thin, flexible electrodes are carefully inserted into the epidural space (the area surrounding the spinal cord).
- Targeted Areas: The electrodes are positioned over specific spinal segments responsible for motor and autonomic functions.
Step 3: Connection to Pulse Generator
- A lead wire from the electrodes is tunneled under the skin and connected to a pulse generator.
- The pulse generator, a small device that controls the electrical impulses, is implanted under the skin, typically in the abdomen or buttocks.
Step 4: Testing and Adjustment
- During the surgery, the electrodes are tested to ensure correct placement and functionality.
- The surgeon and a neurologist may work together to confirm that the stimulation activates the desired spinal cord regions.
3. Post-Placement Programming
a. Initial Programming
- After the device is implanted, it is programmed using an external controller.
- The settings are customized to the patient’s specific needs, targeting motor control, bladder and bowel regulation, or other autonomic functions.
b. Calibration
- The stimulation intensity, frequency, and patterns are adjusted over several sessions post-surgery to achieve optimal results.
4. Closing the Incisions
a. Securing the Device
- The electrodes and pulse generator are secured in place to prevent movement.
b. Suturing
- The incisions are closed using sutures or surgical staples and covered with sterile dressings.
5. Postoperative Monitoring
a. Recovery Room
- The patient is moved to a recovery room for close monitoring of vital signs and surgical site.
b. Initial Testing
- The stimulation device is tested again post-surgery to confirm proper functioning.
c. Pain Management
- Pain medications may be administered to manage post-surgical discomfort.
6. Follow-Up and Rehabilitation
a. Regular Follow-Ups
- Follow-up appointments are scheduled to monitor the patient’s recovery and adjust device settings as needed.
b. Physical Therapy
- Patients participate in a customized rehabilitation program to maximize the benefits of the epidural stimulation.
- Therapy focuses on relearning movements and improving strength and coordination.
c. Device Management
- Patients are trained on how to use the external controller to adjust settings and manage stimulation sessions.
Key Goals of the Procedure
- Restoration of Motor Functions
- Activate dormant neural circuits to facilitate voluntary movements.
- Improvement in Autonomic Functions
- Enhance bladder and bowel control, sexual function, and cardiovascular stability.
- Reduction in Secondary Complications
- Improve circulation, reduce pressure sores, and prevent muscle atrophy.
Duration of the Surgery
The entire procedure typically takes 2 to 4 hours, depending on the complexity of the case and the number of electrodes being implanted.
Risks and Complications
Although the surgery is generally safe, potential risks include:
- Infection at the surgical site.
- Electrode displacement or malfunction.
- Pain or discomfort near the pulse generator.
- Skin irritation over the implanted device.
Conclusion
Epidural stimulation spinal cord injury surgery is a sophisticated and innovative procedure that requires precision and expertise. By directly targeting the spinal cord with electrical stimulation, this technique offers hope to individuals with spinal cord injuries, enabling them to regain motor and autonomic functions that were previously thought to be permanently lost.
post procedure
What will be the postcare of Epidural Stimulation Spinal Cord Injury Surgery patient?
Post care for Epidural Stimulation Spinal Cord Injury Surgery Patients
Postoperative care is a critical phase in the recovery process following epidural stimulation spinal cord injury surgery. It involves medical supervision, lifestyle adjustments, and rehabilitation to ensure optimal healing, proper functioning of the implanted device, and the best possible outcomes for regaining motor and autonomic functions.
1. Immediate Postoperative Care
a. Hospital Stay
- Duration: Patients typically stay in the hospital for 2–5 days for initial monitoring.
- Vital Signs Monitoring: Blood pressure, heart rate, and other vital signs are closely observed.
- Pain Management: Medications such as analgesics are administered to manage surgical discomfort.
b. Wound Care
- Surgical sites (incisions for electrodes and pulse generator) are checked daily for signs of infection or bleeding.
- Dressings are changed as per the surgeon's instructions.
c. Device Function Testing
- The implanted device is tested to ensure proper electrode placement and functioning.
- Adjustments may be made to initial stimulation settings.
2. Discharge Instructions
a. Medication Management
- Painkillers and antibiotics are prescribed to prevent discomfort and infections.
- Patients should follow a strict medication schedule.
b. Physical Activity Restrictions
- Avoid strenuous activities, heavy lifting, or twisting motions for 4–6 weeks to allow proper healing of the surgical site.
- Gradual mobility improvements are encouraged with the guidance of a healthcare provider.
c. Incision Care
- Keep the surgical sites clean and dry.
- Avoid soaking in baths or swimming pools until the incisions are fully healed.
- Watch for signs of infection, such as redness, swelling, or discharge, and report them to the doctor immediately.
3. Follow-Up Appointments
a. Wound Check
- Scheduled 1–2 weeks after surgery to assess incision healing.
- Sutures or staples, if present, are removed during this visit.
b. Device Programming
- The device settings are fine-tuned in follow-up appointments based on patient feedback and responses.
- Adjustments are aimed at optimizing stimulation for desired motor or autonomic improvements.
4. Rehabilitation Therapy
Rehabilitation plays a vital role in enhancing the outcomes of epidural stimulation surgery. A multidisciplinary team, including physical therapists, occupational therapists, and neurologists, supports the recovery process.
a. Physical Therapy
- Focuses on regaining strength, flexibility, and coordination.
- Exercises are designed to improve voluntary movements in areas affected by the spinal cord injury.
b. Gait Training
- If the patient shows progress in lower limb movements, walking exercises with assistive devices may be introduced.
- Therapists provide guidance on safe mobility techniques.
c. Autonomic Function Training
- Patients may undergo training to improve bowel and bladder control, manage blood pressure, and enhance sexual functions.
5. Long-Term Device Management
a. Using the External Controller
- Patients are taught how to operate the external controller to adjust stimulation levels as needed.
- Training includes turning the device on and off and understanding how to respond to changes in stimulation effects.
b. Regular Maintenance
- Periodic check-ups are scheduled to assess the device’s functionality and battery life.
- Battery replacement for the pulse generator may be required every 5–10 years, depending on usage.
c. Troubleshooting
- Patients are advised to report any unusual sensations, reduced stimulation effectiveness, or discomfort near the device to their healthcare provider.
6. Lifestyle Adjustments
a. Diet and Nutrition
- A balanced diet is recommended to support overall healing and recovery.
- High-fiber foods and adequate hydration help maintain bowel health, especially if autonomic functions are affected.
b. Hygiene and Skin Care
- Prevent pressure sores by changing positions frequently and using supportive cushions or mattresses.
- Maintain good hygiene, especially around the surgical sites.
c. Stress Management
- Psychological counseling or support groups can help patients cope with the emotional challenges of recovery.
7. Signs of Complications to Watch For
Patients should contact their healthcare provider immediately if they notice:
- Persistent or worsening pain at the surgical site.
- Signs of infection: fever, redness, swelling, or discharge.
- Malfunction of the implanted device, such as loss of stimulation or irregular sensations.
- Difficulty in movement or worsening symptoms.
8. Long-Term Outcomes
a. Functional Improvements
- With consistent rehabilitation and device optimization, many patients experience improvements in motor function, autonomic regulation, and quality of life.
b. Gradual Progress
- Recovery and functional gains may occur gradually over weeks or months as the body adapts to the device and rehabilitation exercises.
c. Lifelong Commitment
- Commitment to follow-up appointments, rehabilitation, and device management is essential for sustained benefits.
success rate
What will be the success rate of Epidural Stimulation Spinal Cord Injury Surgery?
The success rate of epidural stimulation spinal cord injury (SCI) surgery depends on various factors, including the type and severity of the spinal cord injury, the patient's overall health, adherence to post-surgery rehabilitation, and the goals of the treatment. While exact success rates can vary, clinical studies and patient outcomes have demonstrated significant improvements in motor and autonomic functions for many individuals undergoing this procedure.
Key Metrics of Success
1. Motor Function Improvement
- Success Rate: Approximately 60–80% of patients experience meaningful improvements in voluntary movements, particularly in the lower limbs.
- Details:
- Patients with incomplete spinal cord injuries often show greater recovery potential than those with complete injuries.
- Movements may include the ability to flex knees, wiggle toes, or lift legs under controlled conditions.
2. Autonomic Function Restoration
- Success Rate: Up to 70% of patients report improved bladder, bowel, and sexual function.
- Details:
- Enhanced bladder control reduces dependence on catheters.
- Improved bowel control allows for a more regular and independent bowel routine.
- Many patients also experience better regulation of blood pressure and reduced orthostatic hypotension.
3. Reduction in Secondary Complications
- Improved Quality of Life: A high proportion of patients report fewer complications such as pressure sores, muscle atrophy, and poor circulation.
- Success Rate: About 80–90% of patients see improvements in circulation and muscle health with regular use of the stimulation device.
4. Overall Patient Satisfaction
- Satisfaction Rate: Around 85% of patients express satisfaction with the procedure, citing improved independence, mobility, and quality of life.
- Details:
- Psychological benefits, such as reduced anxiety and depression, are often reported due to regained functional abilities.
Factors Influencing Success
-
Type of Injury
- Incomplete Injuries: Higher success rates, as some neural pathways remain intact.
- Complete Injuries: Progress is slower and may require more extensive rehabilitation.
-
Time Since Injury
- Early intervention generally leads to better outcomes, but even patients with long-term injuries have shown improvements.
-
Rehabilitation Commitment
- Patients who actively participate in post-surgery physical therapy and rehabilitation programs tend to achieve better results.
-
Device Programming and Adjustments
- Customization of the stimulation settings to meet individual needs significantly enhances the efficacy of the procedure.
-
Health and Age
- Younger patients and those without additional health complications often experience faster recovery and better results.
Challenges and Limitations
-
Complete Restoration of Function
- While many patients regain some degree of motor or autonomic function, complete recovery is rare, particularly in cases of severe or complete spinal cord injuries.
-
Time for Visible Results
- Functional improvements may take weeks or months of consistent therapy and device adjustments to become evident.
-
Variability in Response
- Not all patients respond equally; some may achieve only minimal improvements.
Clinical Evidence
Several studies and clinical trials have documented the success rates and outcomes of epidural stimulation:
-
Motor Function Recovery
- A study published in Nature Medicine found that 80% of patients with incomplete SCI achieved significant voluntary movement with epidural stimulation and intensive rehabilitation.
-
Autonomic Improvements
- Research by the Christopher & Dana Reeve Foundation reported that 70% of participants experienced improved bladder and bowel control, alongside better blood pressure regulation.
-
Long-Term Benefits
- Follow-up studies have shown that many patients retain their improvements for years, provided they maintain regular use of the stimulation device and follow their rehabilitation plan.
faqs from doctor
FAQ: Epidural Stimulation Spinal Cord Injury Surgery
Epidural stimulation surgery for spinal cord injuries has gained attention for its ability to improve motor and autonomic functions in patients with spinal cord injuries (SCI). Below are some frequently asked questions (FAQs) about the procedure, its benefits, and its cost in India.
1. What is Epidural Stimulation Spinal Cord Injury Surgery?
Answer:
Epidural stimulation involves the implantation of a device that delivers electrical impulses to the lower spinal cord. These impulses help activate neural circuits responsible for movement and autonomic functions, potentially restoring partial voluntary control in individuals with spinal cord injuries.
2. Who is a Candidate for Epidural Stimulation Surgery?
Answer:
This surgery is suitable for individuals with:
- Chronic spinal cord injuries (both complete and incomplete).
- Minimal or no response to conventional therapies.
- A stable health condition to undergo surgery and rehabilitation.
A thorough evaluation by a medical team is necessary to determine eligibility.
3. What Benefits Can Patients Expect?
Answer:
- Improved voluntary motor control in lower limbs.
- Enhanced bladder and bowel function.
- Better blood pressure regulation.
- Increased independence in daily activities.
- Improved quality of life through regained partial mobility.
4. What is the Procedure for Epidural Stimulation Surgery?
Answer:
The procedure involves:
- Preoperative Assessment: Medical tests and evaluations to determine suitability.
- Device Implantation: Electrodes are implanted on the spinal cord, and a pulse generator is placed under the skin.
- Device Programming: The stimulation device is adjusted to the patient’s specific needs.
- Rehabilitation: Post-surgery physical therapy to maximize benefits.
5. What are the Risks and Complications?
Answer:
- Infection at the surgical site.
- Displacement of electrodes or malfunction of the device.
- Temporary pain or discomfort.
- Lack of improvement in some cases.
- Rarely, nerve damage.
These risks are minimized through proper preoperative evaluation, skilled surgical techniques, and postoperative care.
6. How Long Does Recovery Take?
Answer:
Recovery varies by individual, but typically:
- Initial recovery from surgery: 1–2 weeks.
- Rehabilitation and therapy: Ongoing for several months to achieve optimal results.
Patients must adhere to follow-up appointments and rehabilitation programs.
7. Why Choose India for Epidural Stimulation Surgery?
Answer:
India is a preferred destination for this procedure due to:
- Highly skilled surgeons specializing in spinal cord injury treatments.
- Advanced medical facilities with state-of-the-art technology.
- Affordable costs compared to Western countries.
- Comprehensive rehabilitation services.
8. How Much Does Epidural Stimulation Surgery Cost in India?
Answer:
The epidural stimulation surgery cost in India typically ranges from ₹20,00,000 to ₹35,00,000 (approximately USD 25,000 to USD 35,000).
This includes:
- Preoperative evaluation.
- Surgery and hospitalization.
- Cost of the implant (stimulation device).
- Postoperative follow-up and initial rehabilitation.
9. Does Health Insurance Cover Epidural Stimulation Surgery?
Answer:
Coverage depends on the insurance provider and the patient’s policy. Some international insurance plans may cover the procedure if it is medically indicated. Patients are advised to check with their insurance providers for specific coverage details.
10. Which Hospitals in India Offer Epidural Stimulation Surgery?
Answer:
Some of the leading hospitals providing this surgery include:
- IBS Hospital, New Delhi
- Amrita Hospital, New Delhi
- Apollo Hospitals, Chennai/Delhi/Mumbai
- Fortis Hospitals, Bangalore/Gurgaon
- Manipal Hospitals, Bangalore
- Medanta – The Medicity, Gurgaon
- Max Super Specialty Hospital, Delhi
- Kokilaben Dhirubhai Ambani Hospital, Mumbai
11. What Are the Success Rates of the Procedure?
Answer:
- Approximately 60–80% of patients experience significant improvement in motor function.
- Up to 70% report enhanced bladder, bowel, and blood pressure control.
- Success depends on factors like the severity of injury, patient health, and rehabilitation commitment.
12. What Kind of Postoperative Care is Required?
Answer:
- Regular follow-ups to monitor device function and adjust settings.
- Adherence to a customized rehabilitation program.
- Maintaining proper wound care and avoiding strenuous activities during initial recovery.
13. Is the Surgery Permanent?
Answer:
The implanted device is designed to be long-lasting, but the pulse generator may require replacement every 5–10 years, depending on the battery life and usage.
14. How Can I Prepare for the Surgery?
Answer:
Preparation includes:
- Medical evaluations and tests.
- Stopping certain medications as advised.
- Lifestyle changes like quitting smoking and improving overall fitness.
15. How Can I Get Started with Epidural Stimulation Surgery in India?
Answer:
- Consult a Specialist: Contact a hospital with expertise in spinal cord injury treatments.
- Medical Assessment: Provide your medical records for an evaluation.
- Travel Arrangements: Plan your visit with the hospital’s international patient care team if you’re traveling from abroad.
- Plan for Rehabilitation: Set aside time for postoperative therapy in India or your home country.
Top Doctors
Sorry, There is nothing to show!Come back soon.



















