Duration of Treatment
5 to 7 hours of Surgery
Days of Stay
2 months
Anesthesia
General Anesthesia
Cost
80,000 to 10,0000 USD.
How Much Does Left Ventricular Assist Device (LVAD) Surgery Cost in India?
Are you looking for Left Ventricular Assist Device LVAD Surgery Cost in India at an affordable cost? Here, we answer the question and explain how to choose the top doctors for better results.
We have shortlisted the list of the best top 10 Cardiac Hospitals in India and Surgeons in India on the basis of Hospital accreditations, experience & qualification of surgeons, success rates of procedures, and patient testimonials.
- Left Ventricular Assist Device LVAD Surgery Cost in India: 80,000 to 10,0000 USD.
- Hotel Cost Near Hospital - starting from 18 to 50 USD (as per hotel services)
- Food Cost - starting from 20 to 30 USD (per day)
- Miscellaneous cost - 20 USD (per day).
- It's only a rough estimate, final treatment will plan after the new evaluation reports.
- In India, Left Ventricular Assist Device LVAD Surgery Costs in India can vary as per the diagnosis, patient's condition, best cardiac surgeon experience, Implant quality, hospital facilities, and city.
- To make an appointment, learn more about the LVAD, read the below information, or call / WhatsApp/ Viber - our experts to answer at +91 9582708782. Still, have questions? SUBMIT ENQUIRY
Who is the Top 10 Best Left Ventricular Assist Device (LVAD) Surgeon in India?
- DR. NARESH TREHAN - Medant City Hospital
- DR. Y K MISHRA - Manipal Hospital
- DR. Z S MEHARWAL - Fortis Hospital
- DR. RAMJI MEHROTRA - BLK-MAX Hospital
- DR. COL KUMUD RAI - Max Hospital
- DR. AMIT KUMAR CHAURASIA - Artemis Hospital
- DR. MUKESH GOEL - Apollo Hospital
- DR. DEVI SHETTY - Narayana Hospital
- DR. SANDEEP ATTAWAR - KIMS HOSPITAL
- Dr. Dhaval Naik - Marengo Hospital
Which are the Top 10 Left Ventricular Assist Device (LVAD) Surgery Hospitals in India?
- ARTEMIS HOSPITAL
- MANIPAL HOSPITAL
- BLK HOSPITAL
- FORTIS HOSPITAL
- MEDANTA HOSPITAL
- YASHODHA HOSPITAL
- GLOBAL HOSPITAL
- APOLLO HOSPITAL
- JAYPEE HOSPITAL
- SAIFEE HOSPITAL
- NARAYANA HOSPITAL
Why did you choose Peace Medical Tourism?
We are one of the best healthcare services providers with more than 10 years of experience to provide the best treatment at an affordable cost and guide our international patients to choose the top destination as per patient's budget and treatment.
- Comprehensive and 100% transparency.
- Help to Choose the Best Option for LVAD Surgery.
- Very highly skilled surgeon in India team.
- World-class technology for surgery.
- The high success rate of procedures with international standards.
- Affordable Cost of Left Ventricular Assist Device LVAD Surgery in India.
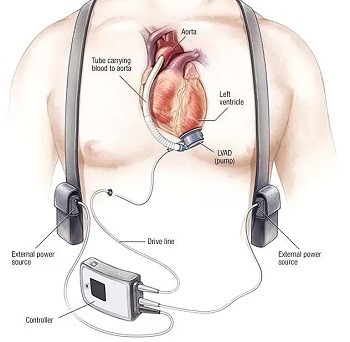
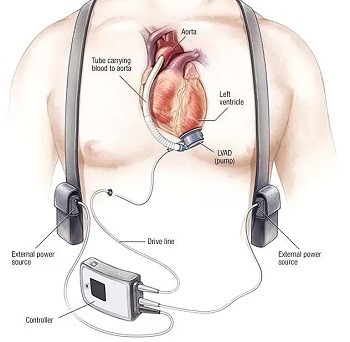
What is a Left Ventricular Assist Device (LVAD)?
- A left ventricular assist device (LVAD) is a mechanical pump that is implanted in the chest. It helps restore normal blood flow in the rest of the body.
- It is used to sustain cardiac function in those with end-stage heart failure or as abridge to heart transplants.
- LVAD can be implanted in one or both ventricles of your heart, but it is most frequently implanted in the left ventricle.
- When placed in the left ventricle, it's called a left ventricular assist device (LVAD).
What types of LVADs are used?
- Heartmate 3 - Is is a circular pump that is implanted into the apex of the heart.
The controller is powered by two batteries or electricity from a wall outlet. - Heartmate 2 - It is a pump that is implanted into the apex of the heart under the muscle layers of the abdomen. The controller is powered by two batteries or electricity from a wall outlet.
Still, have questions? SUBMIT ENQUIRY
What are the symptoms of LVAD patients?
Left Ventricular Assist Device (LVAD) patients can experience a variety of symptoms and signs due to the device itself, the underlying heart condition, or complications related to the LVAD. Below is an overview of common symptoms and observations in LVAD patients:
1. Normal Symptoms
These are typical for LVAD patients and not necessarily concerning:
- No palpable pulse: The continuous flow of most LVADs eliminates the pulse or makes it faint.
- Low blood pressure readings: LVAD patients often have mean arterial pressures (MAPs) between 60-90 mmHg, measured by Doppler.
- Fatigue: Common as patients adapt to the device and manage heart failure.
- Dizziness or lightheadedness: Due to low blood pressure or changes in circulation.
2. Symptoms Indicating Potential Issues
These symptoms may suggest complications and require medical attention:
- Infection signs: Redness, warmth, swelling, or drainage at the driveline exit site, or fever and chills indicating systemic infection.
- Bleeding: Commonly gastrointestinal bleeding due to anticoagulation therapy or acquired von Willebrand syndrome. Symptoms include black or bloody stools, vomiting blood, or unexplained anemia.
- Thromboembolic events: Signs of a stroke, such as sudden weakness, confusion, or difficulty speaking, may indicate a clot formation.
- Pump malfunction: Alarms from the LVAD controller, along with symptoms like fatigue, dizziness, or shortness of breath, may signal a pump issue.
- Heart failure progression: Symptoms such as worsening shortness of breath, fluid retention (swelling in legs or abdomen), and fatigue may indicate right-sided heart failure or insufficient support from the LVAD.
- Arrhythmias: Palpitations, dizziness, or fainting could signal irregular heart rhythms.
- Low flow alarms: Could result from dehydration, hypovolemia, or obstruction within the pump.
3. Emergency Symptoms
These require immediate intervention:
- Sudden shortness of breath or severe chest pain: Potential signs of pump failure, pulmonary embolism, or myocardial infarction.
- Loss of consciousness: Could be due to pump failure, stroke, or severe hypotension.
- Severe bleeding: Especially gastrointestinal or intracranial.
4. Psychological and Emotional Symptoms
- Anxiety and depression: Common due to lifestyle adjustments and concerns about the device.
- Sleep disturbances: Often related to stress or the hum of the device.
5. Device-Related Symptoms
- Driveline discomfort: Mild discomfort at the driveline exit site is normal but should not be accompanied by redness, drainage, or swelling.
- Vibration or noise from the device: May indicate mechanical issues and should be evaluated.
Monitoring and Management
LVAD patients should have regular follow-ups with their healthcare team to monitor:
- Device parameters (flow, speed, power).
- Anticoagulation levels (e.g., INR).
- Signs of complications or device failure.
If symptoms arise, prompt evaluation by a healthcare provider experienced in LVAD management is essential.
What is the Risk Factor of LVAD Surgery?
Left Ventricular Assist Device (LVAD) surgery is a complex procedure with various potential risks. The risks stem from the surgery itself, the patient's underlying health condition, and potential complications related to the device. Below are the key risk factors associated with LVAD surgery:
1. Surgical Risks
- Bleeding:
- The surgery involves significant blood vessel manipulation, and anticoagulation therapy after implantation increases the risk.
- May lead to the need for blood transfusions or reoperation.
- Infection:
- Driveline infections (at the site where the external cable exits the body) are common.
- Sepsis or systemic infections can occur, especially if the infection spreads from the driveline.
- Anesthesia complications:
- Risk of adverse reactions to anesthesia, especially in patients with comorbidities.
2. Device-Related Risks
- Pump thrombosis:
- Blood clots can form in the LVAD, leading to malfunction or embolism.
- Mechanical failure:
- While rare, device malfunction can occur, requiring urgent replacement or repair.
- Driveline complications:
- Driveline fracture, disconnection, or site trauma may occur.
- Low or high pump flow:
- Insufficient or excessive blood flow can lead to hypoperfusion or damage to the heart and other organs.
3. Cardiovascular Risks
- Stroke:
- Both ischemic (caused by clots) and hemorrhagic (caused by bleeding) strokes are significant risks due to anticoagulation therapy and potential embolism.
- Arrhythmias:
- Irregular heart rhythms, including ventricular arrhythmias, are common and can worsen heart function.
- Right-sided heart failure:
- The LVAD supports the left ventricle, but increased blood return to the right ventricle can lead to failure if the right side cannot handle the workload.
- Hypotension or hypertension:
- Imbalances in blood pressure due to pump settings or underlying conditions.
4. Hematologic Risks
- Anticoagulation-related bleeding:
- Lifelong anticoagulation therapy increases the risk of internal bleeding, especially gastrointestinal or intracranial.
- Acquired von Willebrand syndrome:
- Continuous blood flow through the pump can damage clotting factors, increasing bleeding risk.
- Hemolysis:
- Breakdown of red blood cells due to mechanical stress from the device.
5. Pulmonary Risks
- Respiratory complications:
- Prolonged mechanical ventilation, pneumonia, or fluid accumulation in the lungs may occur after surgery.
6. Other Risks
- Organ dysfunction:
- Risk of kidney or liver dysfunction due to low cardiac output, poor perfusion, or complications during surgery.
- Psychological challenges:
- Anxiety, depression, and adjustment disorders can arise due to lifestyle changes and dependency on the device.
- Quality of life issues:
- Managing the external components of the LVAD (e.g., power source, controller) may be challenging.
Risk Factors That Increase Complications
Patients with the following conditions are at higher risk for complications:
- Advanced age.
- Poor general health or malnutrition.
- Significant comorbidities, such as kidney disease, diabetes, or pulmonary hypertension.
- Severe right-sided heart dysfunction.
- History of stroke or bleeding disorders.
- Frailty or immobility.
- Preexisting infection.
Mitigation of Risks
To reduce risks, LVAD candidates typically undergo:
- Thorough preoperative evaluation and optimization of health status.
- Postoperative monitoring in specialized centers.
- Regular follow-ups to manage anticoagulation, monitor device function, and address complications promptly.
LVAD surgery offers life-saving support for patients with advanced heart failure, but the associated risks necessitate careful patient selection and diligent care.
How do you prepare for left ventricular assist device (LVAD) surgery?
- First, you have to choose the best hospital for LVAD Surgery at an affordable cost for better results in India.
- The patient is required to go for PSC ( Pre-surgery check-up ) to do some blood tests, ECG, and ECH for Cardiac check-ups and urine tests to know whether he /she is fit for LVAD surgery or not.
- You’ll be asked to sign a consent form, which gives the surgeon permission to carry out the treatment.
- The doctor should be informed about any medication that the patient may be taking.
- The patient is admitted to the hospital on the same days before the procedures and advised to remain empty stomach/Fasting.
- Thinner's medicines have to stop before ten days of surgery.
- After Angioplasty patients should stay overnight at the hospital.
- LVAD Surgery cost in India is around 80,000 to 10,000 USD the cost varied depending upon the stent quality, city, hospitals, and doctor's experience.
Which are the best Procedures for LVAD Implant Surgery?
Before surgery, the surgeon and anesthesia doctors will guide you about the benefits and risk factors of the LVAD implant.
Step 1 – Anesthesia: A pacemaker usually takes 5 to 7 hours for implantation. The surgeon will give General anesthesia to numb the incision site.
Step 2 – The incision:
- The surgeon will make an incision down your chest and open your chest bone (sternum) to reach your heart and attach the LVAD.
- Open heart surgery is needed to implant an LVAD.
-
During the surgery, the surgeon will use a heart-lung bypass machine to circulate oxygen-rich blood throughout your body during surgery.
-
A breathing machine (ventilator) will take over your breathing during the surgery.
-
Every patient has a different recovery period, and stay in the hospital depends on the patient's condition.
Step 3 – Closing the incisions: The Surgeon will flap the skin with the help of Sutures, skin adhesives, tapes or clips close the incisions after the LVAD implant.
What's the LVAD surgery post-care?
Post-care for Left Ventricular Assist Device (LVAD) surgery is critical to ensure the patient's recovery, maintain device function, and prevent complications. Here's an overview of key aspects of LVAD post-operative care:
1. Immediate Postoperative Care (Hospital Stay)
- Intensive Care Unit (ICU) Monitoring:
- Continuous monitoring of vital signs, LVAD parameters (flow, speed, power), and hemodynamic status.
- Mechanical ventilation support as needed, usually weaned off within 24-48 hours if no complications arise.
- Pain Management:
- Adequate pain control with medications.
- Fluid and Electrolyte Balance:
- Close monitoring of fluid status to avoid dehydration or fluid overload.
- Anticoagulation Therapy:
- Initiation of blood thinners (e.g., heparin or warfarin) to prevent clot formation in the device.
- Regular blood tests to monitor INR (International Normalized Ratio) levels.
- Wound Care:
- Careful attention to surgical incision and driveline exit site to prevent infection.
- Physical Therapy and Mobilization:
- Gradual reintroduction to movement to prevent deconditioning and promote lung function.
2. Transition to Home Care
- Education for Patients and Caregivers:
- Device Management:
- Understanding LVAD equipment, including controller, batteries, and power sources.
- How to respond to alarms and troubleshoot device issues.
- Driveline Care:
- Cleaning and dressing the driveline exit site to prevent infections.
- Anticoagulation Monitoring:
- Recognizing signs of bleeding or clotting and adhering to medication schedules.
- Emergency Preparedness:
- Knowing when to seek medical help, recognizing stroke or pump failure signs.
- Carrying an emergency contact card or device information at all times.
- Device Management:
- Follow-Up Appointments:
- Regular visits to the LVAD clinic for device checks, blood tests, and assessment of overall health.
3. Lifestyle Adjustments
- Diet and Nutrition:
- Low-sodium diet to manage fluid retention and hypertension.
- Adequate hydration to prevent low flow alarms but avoiding overhydration.
- Balanced diet to support wound healing and overall health.
- Physical Activity:
- Gradual increase in activity level as tolerated, under the guidance of a physical therapist.
- Avoiding high-impact activities or activities that could damage the driveline.
- Avoiding Infections:
- Maintaining strict hygiene practices, especially around the driveline.
- Avoiding crowded places or sick individuals during recovery.
4. Psychological and Emotional Support
- Mental Health:
- Addressing anxiety, depression, or stress related to lifestyle changes or living with an LVAD.
- Support groups or counseling for patients and caregivers.
- Social Adjustments:
- Managing daily routines with external components of the LVAD (e.g., power sources, batteries).
5. Long-Term Monitoring and Complication Management
- Regular Checkups:
- Monitoring for signs of infection, bleeding, or device malfunction.
- Device Function:
- Routine evaluation of pump parameters to ensure proper functioning.
- Anticoagulation Therapy:
- Lifelong anticoagulation monitoring to prevent clots or excessive bleeding.
- Management of Comorbidities:
- Optimizing care for conditions such as diabetes, kidney disease, or right heart failure.
- Emergency Situations:
- Recognizing symptoms of complications like stroke, pump thrombosis, or heart failure.
6. Emergency Preparedness
- Ensure the patient always has access to:
- Spare batteries and controller.
- Contact information for the LVAD team and nearest LVAD center.
- Emergency instructions, including protocols for handling power outages.
7. Rehabilitation
- Participation in a cardiac rehabilitation program tailored for LVAD patients to improve physical fitness and quality of life.
Proper post-care for LVAD patients requires a multidisciplinary approach involving cardiologists, surgeons, nurses, physical therapists, and mental health professionals to optimize recovery and long-term outcomes.
What's the Success rate of LVAD?
The success rate of Left Ventricular Assist Device (LVAD) implantation depends on various factors, including the patient's overall health, the underlying cause of heart failure, the surgical center's expertise, and whether the device is being used as a bridge to transplant (BTT), destination therapy (DT), or a bridge to recovery. Here's an overview:
1. General Survival Rates
- 1-Year Survival:
- Approximately 80-85% for patients implanted with contemporary LVADs.
- 2-Year Survival:
- Around 70-75%.
- 5-Year Survival:
- Estimated at 50-60%, depending on patient factors and device type.
2. Factors Affecting Success Rates
Type of Therapy
- Bridge to Transplant (BTT):
- High success rate due to short-term use before a heart transplant.
- Outcomes improve with timely transplant.
- Destination Therapy (DT):
- Used for patients ineligible for transplant.
- Success depends on managing long-term complications and comorbidities.
- Bridge to Recovery:
- Rare; in some cases, the heart may recover enough to allow device removal. Success depends on the underlying cause of heart failure.
Device Type
- Third-generation continuous-flow devices (e.g., HeartMate 3, HeartWare HVAD):
- Superior survival and fewer complications compared to older pulsatile devices.
- Reduced risk of pump thrombosis and mechanical failure.
Patient Factors
- Age: Younger patients tend to have better outcomes.
- Comorbidities: Conditions like kidney disease, diabetes, or right-sided heart failure can reduce success rates.
- Pre-implantation health: Severe malnutrition, infections, or organ dysfunction increase risks.
Center Experience
- High-volume, experienced centers tend to achieve better outcomes due to expertise in patient selection, surgical technique, and postoperative care.
3. Complications That Impact Success
- Infections: Particularly driveline infections, which can lead to sepsis.
- Bleeding: Gastrointestinal bleeding is common due to anticoagulation therapy.
- Stroke: Both ischemic and hemorrhagic strokes are risks.
- Right Heart Failure: Can develop after LVAD implantation.
- Device Malfunctions: Rare with modern devices but still possible.
4. Quality of Life Improvements
- LVADs significantly improve survival and quality of life for patients with advanced heart failure:
- Increased exercise tolerance.
- Reduced heart failure symptoms (e.g., fatigue, breathlessness).
- Better functional status, allowing patients to resume daily activities.
5. Long-Term Outlook
While complications can occur, advancements in LVAD technology and improved patient management continue to enhance survival rates and quality of life. For many patients, LVAD therapy provides a life-saving option when heart failure progresses to end-stage.
What Questions Are Ask before an LVAD implant?
- Are you a board-certified cardiac surgeon for the heart?
- Am I a good patient for you for this procedure?
- Let me know the success rates and how long time will take for recovery.
- What are the risk factors of surgery?
- What treatment plan do you recommend and why?
- What is the Left Ventricular Assist Device LVAD Surgery Cost in India?
- When can I go for normal activities, including exercise?
- Do I have stitches, staples, and/or bandages?
- Do I need any follow-up appointments or tests after my surgery?
- Do your hospitals have the best cardiac intensivist care?
- Does your hospital have the best post-care team?
- Does your hospital have a specialized intensive care unit?
- What are the survival rates of cardiac surgery in your hospital?
Here’s a comprehensive FAQ on Left Ventricular Assist Device (LVAD) Surgery that addresses common questions and concerns about the procedure:
General Questions
What is an LVAD?
An LVAD (Left Ventricular Assist Device) is a mechanical pump implanted in the chest to help the weakened left ventricle of the heart pump blood to the rest of the body. It is used for patients with advanced heart failure.
Who needs an LVAD?
LVADs are typically recommended for:
- Patients awaiting a heart transplant (bridge to transplant).
- Patients ineligible for a transplant but requiring long-term support (destination therapy).
- Patients whose heart may recover enough to potentially remove the device (bridge to recovery).
How does an LVAD work?
The LVAD takes over the pumping function of the left ventricle, delivering blood from the heart to the aorta. Most modern LVADs use continuous flow, meaning they may not produce a detectable pulse.
Before Surgery
What tests are required before LVAD surgery?
Preoperative evaluations typically include:
- Imaging (e.g., echocardiogram, chest X-ray, CT scan).
- Heart catheterization to assess pressures and blood flow.
- Blood tests (kidney function, liver function, clotting ability).
- Psychological and social assessments to ensure readiness for the lifestyle changes.
How do I prepare for the surgery?
- Follow your doctor’s instructions regarding fasting and medications.
- Arrange for a caregiver to assist with recovery and post-surgery care.
- Pack essentials for a hospital stay, including comfortable clothing and personal items.
The Surgery
How is LVAD surgery performed?
The surgery is done under general anesthesia and typically takes 4-6 hours. A surgeon places the pump in the chest, connects it to the heart and aorta, and tunnels the driveline (a cable) through the skin to connect to the external controller and power source.
What are the risks of LVAD surgery?
Risks include:
- Bleeding (due to anticoagulation).
- Infection (especially at the driveline exit site).
- Stroke.
- Right-sided heart failure.
- Device malfunction.
After Surgery
What is the recovery time?
- Hospital stay: 2-4 weeks, depending on complications.
- Full recovery: 2-3 months, with physical therapy and follow-up care.
Will I feel better immediately?
Many patients notice an improvement in energy levels and heart failure symptoms within days or weeks, but full recovery and adjustment to the device take time.
Living with an LVAD
How do I care for the LVAD?
- Keep the driveline site clean and change dressings as instructed.
- Regularly charge and maintain batteries.
- Monitor the controller for alarms and understand how to respond to them.
Can I shower with an LVAD?
Yes, but you’ll need special waterproof equipment to protect the external components. Your healthcare team will provide guidance.
Can I travel with an LVAD?
Yes, but you’ll need to:
- Carry spare batteries, the controller, and a backup power supply.
- Inform airport security about your device.
- Plan for access to an LVAD center near your destination.
Will I need to take medications?
Yes, including:
- Anticoagulants to prevent blood clots.
- Medications to manage other health conditions (e.g., heart failure, blood pressure).
Complications and Follow-Up
What are the signs of complications?
- Signs of infection (redness, swelling, or drainage at the driveline site).
- Stroke symptoms (sudden weakness, difficulty speaking, vision changes).
- Bleeding (e.g., dark stools, vomiting blood).
- Pump alarms or unusual sounds.
How often do I need follow-ups?
Initially, follow-ups are frequent (weekly or bi-weekly) and decrease over time. Regular monitoring is essential for managing the device and overall health.
Lifestyle Questions
Will I have a pulse with an LVAD?
Many LVADs create continuous blood flow, so you may not have a palpable pulse. Blood pressure is monitored using mean arterial pressure (MAP).
Can I exercise with an LVAD?
Yes, light to moderate exercise is encouraged under medical guidance. Avoid high-impact activities or those that could damage the driveline.
Can I have children with an LVAD?
Pregnancy is typically not recommended due to the risks associated with anticoagulation therapy and heart function.
Long-Term Outlook
How long can I live with an LVAD?
With advancements in technology, survival rates have improved:
- 1-year survival: ~80-85%.
- 5-year survival: ~50-60%. Some patients live many years with proper care and management.
Can the LVAD be removed if my heart recovers?
In rare cases, if the heart regains enough strength, the LVAD can be removed. This is called a "bridge to recovery."
Will I still need a heart transplant?
If the LVAD is being used as a bridge to transplant, you will remain on the transplant list.
Costs and Insurance
Is LVAD surgery covered by insurance?
Most insurance plans and Medicare cover LVAD surgery and associated costs, especially if it's deemed medically necessary.
What are the ongoing costs?
Ongoing costs include medications, regular follow-ups, and replacement of external components like batteries and controllers.
Emergency Preparedness
What should I do in an emergency?
- Keep spare batteries and a controller nearby at all times.
- Carry an LVAD emergency contact card with details about your device.
- Contact your LVAD team immediately if issues arise.
What happens if there’s a power outage?
The LVAD has battery backups. Always keep spare, fully charged batteries available and know how to switch power sources.
Top Doctors
Top Hospitals
LVAD SURGERY COST IN INDIA
Duration of Treatment
5 to 7 hours of Surgery
Days of Stay
2 months
Anesthesia
General Anesthesia
Cost
80,000 to 10,0000 USD.
How Much Does Left Ventricular Assist Device (LVAD) Surgery Cost in India?
Are you looking for Left Ventricular Assist Device LVAD Surgery Cost in India at an affordable cost? Here, we answer the question and explain how to choose the top doctors for better results.
We have shortlisted the list of the best top 10 Cardiac Hospitals in India and Surgeons in India on the basis of Hospital accreditations, experience & qualification of surgeons, success rates of procedures, and patient testimonials.
- Left Ventricular Assist Device LVAD Surgery Cost in India: 80,000 to 10,0000 USD.
- Hotel Cost Near Hospital - starting from 18 to 50 USD (as per hotel services)
- Food Cost - starting from 20 to 30 USD (per day)
- Miscellaneous cost - 20 USD (per day).
- It's only a rough estimate, final treatment will plan after the new evaluation reports.
- In India, Left Ventricular Assist Device LVAD Surgery Costs in India can vary as per the diagnosis, patient's condition, best cardiac surgeon experience, Implant quality, hospital facilities, and city.
- To make an appointment, learn more about the LVAD, read the below information, or call / WhatsApp/ Viber - our experts to answer at +91 9582708782. Still, have questions? SUBMIT ENQUIRY
Who is the Top 10 Best Left Ventricular Assist Device (LVAD) Surgeon in India?
- DR. NARESH TREHAN - Medant City Hospital
- DR. Y K MISHRA - Manipal Hospital
- DR. Z S MEHARWAL - Fortis Hospital
- DR. RAMJI MEHROTRA - BLK-MAX Hospital
- DR. COL KUMUD RAI - Max Hospital
- DR. AMIT KUMAR CHAURASIA - Artemis Hospital
- DR. MUKESH GOEL - Apollo Hospital
- DR. DEVI SHETTY - Narayana Hospital
- DR. SANDEEP ATTAWAR - KIMS HOSPITAL
- Dr. Dhaval Naik - Marengo Hospital
Which are the Top 10 Left Ventricular Assist Device (LVAD) Surgery Hospitals in India?
- ARTEMIS HOSPITAL
- MANIPAL HOSPITAL
- BLK HOSPITAL
- FORTIS HOSPITAL
- MEDANTA HOSPITAL
- YASHODHA HOSPITAL
- GLOBAL HOSPITAL
- APOLLO HOSPITAL
- JAYPEE HOSPITAL
- SAIFEE HOSPITAL
- NARAYANA HOSPITAL
Why did you choose Peace Medical Tourism?
We are one of the best healthcare services providers with more than 10 years of experience to provide the best treatment at an affordable cost and guide our international patients to choose the top destination as per patient's budget and treatment.
- Comprehensive and 100% transparency.
- Help to Choose the Best Option for LVAD Surgery.
- Very highly skilled surgeon in India team.
- World-class technology for surgery.
- The high success rate of procedures with international standards.
- Affordable Cost of Left Ventricular Assist Device LVAD Surgery in India.
What is a Left Ventricular Assist Device (LVAD)?
- A left ventricular assist device (LVAD) is a mechanical pump that is implanted in the chest. It helps restore normal blood flow in the rest of the body.
- It is used to sustain cardiac function in those with end-stage heart failure or as abridge to heart transplants.
- LVAD can be implanted in one or both ventricles of your heart, but it is most frequently implanted in the left ventricle.
- When placed in the left ventricle, it's called a left ventricular assist device (LVAD).
What types of LVADs are used?
- Heartmate 3 - Is is a circular pump that is implanted into the apex of the heart.
The controller is powered by two batteries or electricity from a wall outlet. - Heartmate 2 - It is a pump that is implanted into the apex of the heart under the muscle layers of the abdomen. The controller is powered by two batteries or electricity from a wall outlet.
Still, have questions? SUBMIT ENQUIRY
symptoms
What are the symptoms of LVAD patients?
Left Ventricular Assist Device (LVAD) patients can experience a variety of symptoms and signs due to the device itself, the underlying heart condition, or complications related to the LVAD. Below is an overview of common symptoms and observations in LVAD patients:
1. Normal Symptoms
These are typical for LVAD patients and not necessarily concerning:
- No palpable pulse: The continuous flow of most LVADs eliminates the pulse or makes it faint.
- Low blood pressure readings: LVAD patients often have mean arterial pressures (MAPs) between 60-90 mmHg, measured by Doppler.
- Fatigue: Common as patients adapt to the device and manage heart failure.
- Dizziness or lightheadedness: Due to low blood pressure or changes in circulation.
2. Symptoms Indicating Potential Issues
These symptoms may suggest complications and require medical attention:
- Infection signs: Redness, warmth, swelling, or drainage at the driveline exit site, or fever and chills indicating systemic infection.
- Bleeding: Commonly gastrointestinal bleeding due to anticoagulation therapy or acquired von Willebrand syndrome. Symptoms include black or bloody stools, vomiting blood, or unexplained anemia.
- Thromboembolic events: Signs of a stroke, such as sudden weakness, confusion, or difficulty speaking, may indicate a clot formation.
- Pump malfunction: Alarms from the LVAD controller, along with symptoms like fatigue, dizziness, or shortness of breath, may signal a pump issue.
- Heart failure progression: Symptoms such as worsening shortness of breath, fluid retention (swelling in legs or abdomen), and fatigue may indicate right-sided heart failure or insufficient support from the LVAD.
- Arrhythmias: Palpitations, dizziness, or fainting could signal irregular heart rhythms.
- Low flow alarms: Could result from dehydration, hypovolemia, or obstruction within the pump.
3. Emergency Symptoms
These require immediate intervention:
- Sudden shortness of breath or severe chest pain: Potential signs of pump failure, pulmonary embolism, or myocardial infarction.
- Loss of consciousness: Could be due to pump failure, stroke, or severe hypotension.
- Severe bleeding: Especially gastrointestinal or intracranial.
4. Psychological and Emotional Symptoms
- Anxiety and depression: Common due to lifestyle adjustments and concerns about the device.
- Sleep disturbances: Often related to stress or the hum of the device.
5. Device-Related Symptoms
- Driveline discomfort: Mild discomfort at the driveline exit site is normal but should not be accompanied by redness, drainage, or swelling.
- Vibration or noise from the device: May indicate mechanical issues and should be evaluated.
Monitoring and Management
LVAD patients should have regular follow-ups with their healthcare team to monitor:
- Device parameters (flow, speed, power).
- Anticoagulation levels (e.g., INR).
- Signs of complications or device failure.
If symptoms arise, prompt evaluation by a healthcare provider experienced in LVAD management is essential.
risk factors
What is the Risk Factor of LVAD Surgery?
Left Ventricular Assist Device (LVAD) surgery is a complex procedure with various potential risks. The risks stem from the surgery itself, the patient's underlying health condition, and potential complications related to the device. Below are the key risk factors associated with LVAD surgery:
1. Surgical Risks
- Bleeding:
- The surgery involves significant blood vessel manipulation, and anticoagulation therapy after implantation increases the risk.
- May lead to the need for blood transfusions or reoperation.
- Infection:
- Driveline infections (at the site where the external cable exits the body) are common.
- Sepsis or systemic infections can occur, especially if the infection spreads from the driveline.
- Anesthesia complications:
- Risk of adverse reactions to anesthesia, especially in patients with comorbidities.
2. Device-Related Risks
- Pump thrombosis:
- Blood clots can form in the LVAD, leading to malfunction or embolism.
- Mechanical failure:
- While rare, device malfunction can occur, requiring urgent replacement or repair.
- Driveline complications:
- Driveline fracture, disconnection, or site trauma may occur.
- Low or high pump flow:
- Insufficient or excessive blood flow can lead to hypoperfusion or damage to the heart and other organs.
3. Cardiovascular Risks
- Stroke:
- Both ischemic (caused by clots) and hemorrhagic (caused by bleeding) strokes are significant risks due to anticoagulation therapy and potential embolism.
- Arrhythmias:
- Irregular heart rhythms, including ventricular arrhythmias, are common and can worsen heart function.
- Right-sided heart failure:
- The LVAD supports the left ventricle, but increased blood return to the right ventricle can lead to failure if the right side cannot handle the workload.
- Hypotension or hypertension:
- Imbalances in blood pressure due to pump settings or underlying conditions.
4. Hematologic Risks
- Anticoagulation-related bleeding:
- Lifelong anticoagulation therapy increases the risk of internal bleeding, especially gastrointestinal or intracranial.
- Acquired von Willebrand syndrome:
- Continuous blood flow through the pump can damage clotting factors, increasing bleeding risk.
- Hemolysis:
- Breakdown of red blood cells due to mechanical stress from the device.
5. Pulmonary Risks
- Respiratory complications:
- Prolonged mechanical ventilation, pneumonia, or fluid accumulation in the lungs may occur after surgery.
6. Other Risks
- Organ dysfunction:
- Risk of kidney or liver dysfunction due to low cardiac output, poor perfusion, or complications during surgery.
- Psychological challenges:
- Anxiety, depression, and adjustment disorders can arise due to lifestyle changes and dependency on the device.
- Quality of life issues:
- Managing the external components of the LVAD (e.g., power source, controller) may be challenging.
Risk Factors That Increase Complications
Patients with the following conditions are at higher risk for complications:
- Advanced age.
- Poor general health or malnutrition.
- Significant comorbidities, such as kidney disease, diabetes, or pulmonary hypertension.
- Severe right-sided heart dysfunction.
- History of stroke or bleeding disorders.
- Frailty or immobility.
- Preexisting infection.
Mitigation of Risks
To reduce risks, LVAD candidates typically undergo:
- Thorough preoperative evaluation and optimization of health status.
- Postoperative monitoring in specialized centers.
- Regular follow-ups to manage anticoagulation, monitor device function, and address complications promptly.
LVAD surgery offers life-saving support for patients with advanced heart failure, but the associated risks necessitate careful patient selection and diligent care.
preparation
How do you prepare for left ventricular assist device (LVAD) surgery?
- First, you have to choose the best hospital for LVAD Surgery at an affordable cost for better results in India.
- The patient is required to go for PSC ( Pre-surgery check-up ) to do some blood tests, ECG, and ECH for Cardiac check-ups and urine tests to know whether he /she is fit for LVAD surgery or not.
- You’ll be asked to sign a consent form, which gives the surgeon permission to carry out the treatment.
- The doctor should be informed about any medication that the patient may be taking.
- The patient is admitted to the hospital on the same days before the procedures and advised to remain empty stomach/Fasting.
- Thinner's medicines have to stop before ten days of surgery.
- After Angioplasty patients should stay overnight at the hospital.
- LVAD Surgery cost in India is around 80,000 to 10,000 USD the cost varied depending upon the stent quality, city, hospitals, and doctor's experience.
procedure
Which are the best Procedures for LVAD Implant Surgery?
Before surgery, the surgeon and anesthesia doctors will guide you about the benefits and risk factors of the LVAD implant.
Step 1 – Anesthesia: A pacemaker usually takes 5 to 7 hours for implantation. The surgeon will give General anesthesia to numb the incision site.
Step 2 – The incision:
- The surgeon will make an incision down your chest and open your chest bone (sternum) to reach your heart and attach the LVAD.
- Open heart surgery is needed to implant an LVAD.
-
During the surgery, the surgeon will use a heart-lung bypass machine to circulate oxygen-rich blood throughout your body during surgery.
-
A breathing machine (ventilator) will take over your breathing during the surgery.
-
Every patient has a different recovery period, and stay in the hospital depends on the patient's condition.
Step 3 – Closing the incisions: The Surgeon will flap the skin with the help of Sutures, skin adhesives, tapes or clips close the incisions after the LVAD implant.
post procedure
What's the LVAD surgery post-care?
Post-care for Left Ventricular Assist Device (LVAD) surgery is critical to ensure the patient's recovery, maintain device function, and prevent complications. Here's an overview of key aspects of LVAD post-operative care:
1. Immediate Postoperative Care (Hospital Stay)
- Intensive Care Unit (ICU) Monitoring:
- Continuous monitoring of vital signs, LVAD parameters (flow, speed, power), and hemodynamic status.
- Mechanical ventilation support as needed, usually weaned off within 24-48 hours if no complications arise.
- Pain Management:
- Adequate pain control with medications.
- Fluid and Electrolyte Balance:
- Close monitoring of fluid status to avoid dehydration or fluid overload.
- Anticoagulation Therapy:
- Initiation of blood thinners (e.g., heparin or warfarin) to prevent clot formation in the device.
- Regular blood tests to monitor INR (International Normalized Ratio) levels.
- Wound Care:
- Careful attention to surgical incision and driveline exit site to prevent infection.
- Physical Therapy and Mobilization:
- Gradual reintroduction to movement to prevent deconditioning and promote lung function.
2. Transition to Home Care
- Education for Patients and Caregivers:
- Device Management:
- Understanding LVAD equipment, including controller, batteries, and power sources.
- How to respond to alarms and troubleshoot device issues.
- Driveline Care:
- Cleaning and dressing the driveline exit site to prevent infections.
- Anticoagulation Monitoring:
- Recognizing signs of bleeding or clotting and adhering to medication schedules.
- Emergency Preparedness:
- Knowing when to seek medical help, recognizing stroke or pump failure signs.
- Carrying an emergency contact card or device information at all times.
- Device Management:
- Follow-Up Appointments:
- Regular visits to the LVAD clinic for device checks, blood tests, and assessment of overall health.
3. Lifestyle Adjustments
- Diet and Nutrition:
- Low-sodium diet to manage fluid retention and hypertension.
- Adequate hydration to prevent low flow alarms but avoiding overhydration.
- Balanced diet to support wound healing and overall health.
- Physical Activity:
- Gradual increase in activity level as tolerated, under the guidance of a physical therapist.
- Avoiding high-impact activities or activities that could damage the driveline.
- Avoiding Infections:
- Maintaining strict hygiene practices, especially around the driveline.
- Avoiding crowded places or sick individuals during recovery.
4. Psychological and Emotional Support
- Mental Health:
- Addressing anxiety, depression, or stress related to lifestyle changes or living with an LVAD.
- Support groups or counseling for patients and caregivers.
- Social Adjustments:
- Managing daily routines with external components of the LVAD (e.g., power sources, batteries).
5. Long-Term Monitoring and Complication Management
- Regular Checkups:
- Monitoring for signs of infection, bleeding, or device malfunction.
- Device Function:
- Routine evaluation of pump parameters to ensure proper functioning.
- Anticoagulation Therapy:
- Lifelong anticoagulation monitoring to prevent clots or excessive bleeding.
- Management of Comorbidities:
- Optimizing care for conditions such as diabetes, kidney disease, or right heart failure.
- Emergency Situations:
- Recognizing symptoms of complications like stroke, pump thrombosis, or heart failure.
6. Emergency Preparedness
- Ensure the patient always has access to:
- Spare batteries and controller.
- Contact information for the LVAD team and nearest LVAD center.
- Emergency instructions, including protocols for handling power outages.
7. Rehabilitation
- Participation in a cardiac rehabilitation program tailored for LVAD patients to improve physical fitness and quality of life.
Proper post-care for LVAD patients requires a multidisciplinary approach involving cardiologists, surgeons, nurses, physical therapists, and mental health professionals to optimize recovery and long-term outcomes.
success rate
What's the Success rate of LVAD?
The success rate of Left Ventricular Assist Device (LVAD) implantation depends on various factors, including the patient's overall health, the underlying cause of heart failure, the surgical center's expertise, and whether the device is being used as a bridge to transplant (BTT), destination therapy (DT), or a bridge to recovery. Here's an overview:
1. General Survival Rates
- 1-Year Survival:
- Approximately 80-85% for patients implanted with contemporary LVADs.
- 2-Year Survival:
- Around 70-75%.
- 5-Year Survival:
- Estimated at 50-60%, depending on patient factors and device type.
2. Factors Affecting Success Rates
Type of Therapy
- Bridge to Transplant (BTT):
- High success rate due to short-term use before a heart transplant.
- Outcomes improve with timely transplant.
- Destination Therapy (DT):
- Used for patients ineligible for transplant.
- Success depends on managing long-term complications and comorbidities.
- Bridge to Recovery:
- Rare; in some cases, the heart may recover enough to allow device removal. Success depends on the underlying cause of heart failure.
Device Type
- Third-generation continuous-flow devices (e.g., HeartMate 3, HeartWare HVAD):
- Superior survival and fewer complications compared to older pulsatile devices.
- Reduced risk of pump thrombosis and mechanical failure.
Patient Factors
- Age: Younger patients tend to have better outcomes.
- Comorbidities: Conditions like kidney disease, diabetes, or right-sided heart failure can reduce success rates.
- Pre-implantation health: Severe malnutrition, infections, or organ dysfunction increase risks.
Center Experience
- High-volume, experienced centers tend to achieve better outcomes due to expertise in patient selection, surgical technique, and postoperative care.
3. Complications That Impact Success
- Infections: Particularly driveline infections, which can lead to sepsis.
- Bleeding: Gastrointestinal bleeding is common due to anticoagulation therapy.
- Stroke: Both ischemic and hemorrhagic strokes are risks.
- Right Heart Failure: Can develop after LVAD implantation.
- Device Malfunctions: Rare with modern devices but still possible.
4. Quality of Life Improvements
- LVADs significantly improve survival and quality of life for patients with advanced heart failure:
- Increased exercise tolerance.
- Reduced heart failure symptoms (e.g., fatigue, breathlessness).
- Better functional status, allowing patients to resume daily activities.
5. Long-Term Outlook
While complications can occur, advancements in LVAD technology and improved patient management continue to enhance survival rates and quality of life. For many patients, LVAD therapy provides a life-saving option when heart failure progresses to end-stage.
faqs from doctor
What Questions Are Ask before an LVAD implant?
- Are you a board-certified cardiac surgeon for the heart?
- Am I a good patient for you for this procedure?
- Let me know the success rates and how long time will take for recovery.
- What are the risk factors of surgery?
- What treatment plan do you recommend and why?
- What is the Left Ventricular Assist Device LVAD Surgery Cost in India?
- When can I go for normal activities, including exercise?
- Do I have stitches, staples, and/or bandages?
- Do I need any follow-up appointments or tests after my surgery?
- Do your hospitals have the best cardiac intensivist care?
- Does your hospital have the best post-care team?
- Does your hospital have a specialized intensive care unit?
- What are the survival rates of cardiac surgery in your hospital?
Here’s a comprehensive FAQ on Left Ventricular Assist Device (LVAD) Surgery that addresses common questions and concerns about the procedure:
General Questions
What is an LVAD?
An LVAD (Left Ventricular Assist Device) is a mechanical pump implanted in the chest to help the weakened left ventricle of the heart pump blood to the rest of the body. It is used for patients with advanced heart failure.
Who needs an LVAD?
LVADs are typically recommended for:
- Patients awaiting a heart transplant (bridge to transplant).
- Patients ineligible for a transplant but requiring long-term support (destination therapy).
- Patients whose heart may recover enough to potentially remove the device (bridge to recovery).
How does an LVAD work?
The LVAD takes over the pumping function of the left ventricle, delivering blood from the heart to the aorta. Most modern LVADs use continuous flow, meaning they may not produce a detectable pulse.
Before Surgery
What tests are required before LVAD surgery?
Preoperative evaluations typically include:
- Imaging (e.g., echocardiogram, chest X-ray, CT scan).
- Heart catheterization to assess pressures and blood flow.
- Blood tests (kidney function, liver function, clotting ability).
- Psychological and social assessments to ensure readiness for the lifestyle changes.
How do I prepare for the surgery?
- Follow your doctor’s instructions regarding fasting and medications.
- Arrange for a caregiver to assist with recovery and post-surgery care.
- Pack essentials for a hospital stay, including comfortable clothing and personal items.
The Surgery
How is LVAD surgery performed?
The surgery is done under general anesthesia and typically takes 4-6 hours. A surgeon places the pump in the chest, connects it to the heart and aorta, and tunnels the driveline (a cable) through the skin to connect to the external controller and power source.
What are the risks of LVAD surgery?
Risks include:
- Bleeding (due to anticoagulation).
- Infection (especially at the driveline exit site).
- Stroke.
- Right-sided heart failure.
- Device malfunction.
After Surgery
What is the recovery time?
- Hospital stay: 2-4 weeks, depending on complications.
- Full recovery: 2-3 months, with physical therapy and follow-up care.
Will I feel better immediately?
Many patients notice an improvement in energy levels and heart failure symptoms within days or weeks, but full recovery and adjustment to the device take time.
Living with an LVAD
How do I care for the LVAD?
- Keep the driveline site clean and change dressings as instructed.
- Regularly charge and maintain batteries.
- Monitor the controller for alarms and understand how to respond to them.
Can I shower with an LVAD?
Yes, but you’ll need special waterproof equipment to protect the external components. Your healthcare team will provide guidance.
Can I travel with an LVAD?
Yes, but you’ll need to:
- Carry spare batteries, the controller, and a backup power supply.
- Inform airport security about your device.
- Plan for access to an LVAD center near your destination.
Will I need to take medications?
Yes, including:
- Anticoagulants to prevent blood clots.
- Medications to manage other health conditions (e.g., heart failure, blood pressure).
Complications and Follow-Up
What are the signs of complications?
- Signs of infection (redness, swelling, or drainage at the driveline site).
- Stroke symptoms (sudden weakness, difficulty speaking, vision changes).
- Bleeding (e.g., dark stools, vomiting blood).
- Pump alarms or unusual sounds.
How often do I need follow-ups?
Initially, follow-ups are frequent (weekly or bi-weekly) and decrease over time. Regular monitoring is essential for managing the device and overall health.
Lifestyle Questions
Will I have a pulse with an LVAD?
Many LVADs create continuous blood flow, so you may not have a palpable pulse. Blood pressure is monitored using mean arterial pressure (MAP).
Can I exercise with an LVAD?
Yes, light to moderate exercise is encouraged under medical guidance. Avoid high-impact activities or those that could damage the driveline.
Can I have children with an LVAD?
Pregnancy is typically not recommended due to the risks associated with anticoagulation therapy and heart function.
Long-Term Outlook
How long can I live with an LVAD?
With advancements in technology, survival rates have improved:
- 1-year survival: ~80-85%.
- 5-year survival: ~50-60%. Some patients live many years with proper care and management.
Can the LVAD be removed if my heart recovers?
In rare cases, if the heart regains enough strength, the LVAD can be removed. This is called a "bridge to recovery."
Will I still need a heart transplant?
If the LVAD is being used as a bridge to transplant, you will remain on the transplant list.
Costs and Insurance
Is LVAD surgery covered by insurance?
Most insurance plans and Medicare cover LVAD surgery and associated costs, especially if it's deemed medically necessary.
What are the ongoing costs?
Ongoing costs include medications, regular follow-ups, and replacement of external components like batteries and controllers.
Emergency Preparedness
What should I do in an emergency?
- Keep spare batteries and a controller nearby at all times.
- Carry an LVAD emergency contact card with details about your device.
- Contact your LVAD team immediately if issues arise.
What happens if there’s a power outage?
The LVAD has battery backups. Always keep spare, fully charged batteries available and know how to switch power sources.