Duration of Treatment
usually takes 4 to 5 hours.
Days of Stay
usually 3 to 5 days in the hospital and 30 days outside the hospital.
Anesthesia
Local and General Anesthesia.
Cost
22,000 to 28,000 USD
How much does Deep Brain Stimulation Surgery (DBS) Cost in India?
"Looking for Deep Brain Stimulation Surgery Cost in India or Best Neurosurgeon at an affordable cost in different cities like Delhi, Mumbai, Chennai, Kolkata, and Bangalore? Here, we answer the question and explain how to choose the best neuro hospital list for better results.
We have also shortlisted the list of best top Hospitals and Surgeons on the basis of Hospital accreditations, experience & qualification of surgeons, success rates of procedures, and patient testimonials.
- Deep Brain Stimulation Surgery Cost in India : Starting from 22,000 to 28,000 USD
- Hotel Cost Near Hospital - starting from 18 to 50 USD ( as per hotel services)
- Food Cost - starting from 20 to 30 USD (per day )
- Miscellaneous cost - 20 USD (per day)
- It's an only rough estimate, final treatment will plan after the fresh evaluation reports.
- Deep Brain Stimulation Surgery Cost in India can vary as per the diagnosis, patient conditions, surgeon experience, Implant quality, hospital facilities, and city.
- To make an appointment, learn more about brian, read below information, or call / WhatsApp/ Viber - our experts to answer at +91 9582708782. Still, have questions? SUBMIT ENQUIRY
Who is the Top Best NeuroSurgeon in India?
- Dr. Bipin Walia
- Dr. Rana Patir
- Dr. Anil Kumar Kansa
- Dr. Vikas Gupta
- Dr. Aditya Gupta
- Dr. Sunit Mediratta
- Dr. Rahul Gupta
- Dr. Arun Saroha
- Dr. Anandh Balasubramaniam
- Dr. Shibu Vasudevan Pillai
Which is the Best DBS Hospital in India?
- ARTEMIS HOSPITAL
- MANIPAL HOSPITAL
- BLK HOSPITAL
- APOLLO HOSPITAL
- FORTIS HOSPITAL
- MAX HOSPITAL
- MEDANTA HOSPITAL
- YASHODHA HOSPITAL
- GLOBAL HOSPITAL
- NARAYANA HOSPITAL
Why did you choose Peace Medical Tourism?
We are one of the best healthcare services providers with more than 10 years of experience in providing the best treatment at an affordable cost and guide our international patients to choose the top destination as per patient's budget and treatment.
- Comprehensive and 100% transparency.
- Help to Choose the Best Option for Treatment.
- Very highly skilled Neurosurgeon in India team.
- World-class technology for surgery.
- The high success rate of procedures with international standards.
- Affordable Cost of DBS surgery.
What is Deep Brain Stimulation?
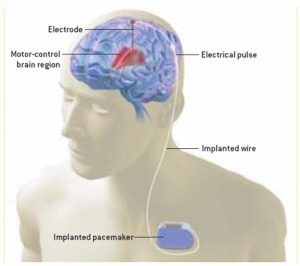
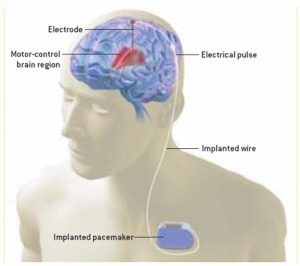
Deep brain stimulation (DBS) is a surgical procedure that involves implanting an electrode device called a brain pacemaker, to send electrical impulses to the areas of the brain that control movement, pain, mood, weight, and awakening. Deep brain stimulation is used to treat, Essential tremors, Parkinson's disease, Tourette syndrome, Chronic Pain, Dystonia, and Epilepsy.
Types of Deep Brain Stimulation:-
- Subthalamic DBS
- Globus pallidus DBS
- Thalamic DBS
- Pedunculopontine nucleus DBS
Still, have questions? SUBMIT ENQUIRY
What are the Signs and Symptoms of Deep brain stimulation (DBS) surgery?
- Essential tremor
- Multiple sclerosis
- Dystonia
- Psychiatric conditions
- Alzheimer’s disease
What are the risk factors of Deep brain stimulation (DBS) surgery?
- Bleeding in the brain
- Stroke
- Brain swelling
- Vision and speech defect
- Infection
- Coma
- Breathing problems
- Nausea
- Heart problems
- Seizures
How to Prepare yourself for Deep brain stimulation (DBS) surgery?
- First, you have to choose the Best neuro hospitals in India or abroad and a top neurosurgeon at an affordable cost for better results.
- The patient is required to go for PSC ( Pre-surgery check-up ) to do some blood test, ECG and ECH for Cardiac check-up and urine tests to know he /she is fit for surgery or not.
- Comprehensive Assessment: The patient undergoes neurological evaluations, imaging (MRI or CT scans), and psychological assessments to confirm suitability for DBS.
- Identifying Target Areas: Based on the disorder, specific brain areas such as the subthalamic nucleus (STN), globus pallidus interna (GPi), or thalamus are selected for stimulation.
- Before the operation, you’ll be asked to sign a consent form, which gives the surgeon permission to carry out the treatment.
- The doctor should be informed about any medication that the patient may be taking.
- The patient is admitted to the hospital on the same days before the procedures and advised to remain empty stomach/Fasting.
- Thinners medicines have to stop before ten days of surgery.
What is the Procedure for Deep brain stimulation (DBS) surgery?
To identify the diagnosis doctor advised to go for complete evolution - usually, blood investigation, (CT) scans, magnetic resonance (MRI) imaging for brain-imaging studies, angiography (imaging the brain's blood vessels), and ventriculography (imaging the brain's ventricles). Before surgery, the surgeon and anesthesia will guide you about the benefits and risk factors of Deep brain stimulation (DBS) surgery.
Step 1 – Anesthesia: Deep brain stimulation (DBS) surgery takes 4 to 5 hours depending upon the procedures by giving local or general anesthesia to relieve pain.
Step 2 – The incision: Deep brain stimulation surgery is usually done in two stages.
- First Stage (Brain surgery) - The patient will go under local anesthesia. The patient’s head is placed in a rigid frame using small screws is called frame-based stereotaxis. And the neurosurgeon makes a small hole into the skull to insert a thin wire lead and will place in a particular part of the brain. A wire goes under the skin and pulse generator implanted near the collarbone.
Surgical Preparation
- Stereotactic Frame Placement: A lightweight frame is attached to the patient’s head under local anesthesia to provide precise coordinates for targeting the brain.
- Imaging for Target Localization: An MRI or CT scan is performed to map the brain and identify the exact location of the target area.
mplanting the Electrodes
- Procedure Type: Usually performed under local anesthesia so the patient can provide feedback to assess symptom improvement during surgery.
- Drilling Small Holes: Small holes are drilled into the skull to access the brain.
- Electrode Placement: Thin, insulated wires (electrodes) are inserted into the target area of the brain using a stereotactic system for precision.
- Intraoperative Testing: Temporary stimulation is performed to confirm the electrodes are correctly placed by observing symptom reduction or monitoring brain responses.
Implanting the Neurostimulator
- General Anesthesia: Once the electrodes are placed, the patient is typically put under general anesthesia.
- Pulse Generator Placement: A small device called a neurostimulator (similar to a pacemaker) is implanted under the skin, usually in the chest or abdomen.
- Connecting Wires: Leads from the brain electrodes are tunneled under the skin and connected to the neurostimulator.
- Second Stage (Chest wall surgery) - The patient will go under General anesthesia. A small incision is made below the collarbone. A wire goes under the skin and pulse generator implanted near the collarbone. This extension of thin wire connects the electrode to the neurostimulator and is programmed to send continuous electrical pulses to your brain.
Step 3 – Closing the incisions: The neurosurgeon flaps the skin after the surgery with the help of Sutures, skin adhesives, tapes or clips that close the skin incisions.
What is the Post care for Deep brain stimulation (DBS)?
The doctor will give complete information about post care of surgery, regarding recovery; proper caring of incisions, taking medications, and managing. Stitches or staples will be removed after a few days of surgery. The batteries of the neurostimulator need to be changed in 3 to 5 years.
Post-Surgical Programming
- Device Activation: A few weeks after surgery, the neurostimulator is activated and programmed by a neurologist or movement disorder specialist.
- Adjusting Settings: The device’s electrical pulses are fine-tuned to optimize symptom control while minimizing side effects.
Additional Considerations
- Adjustable and Reversible: DBS does not destroy brain tissue, and the settings can be modified or turned off if necessary.
- Battery Replacement: Depending on the device type, the neurostimulator battery may need replacement every 3–5 years (non-rechargeable) or recharging at regular intervals (rechargeable).
his step-by-step procedure ensures a personalized and precise approach to improving symptoms and enhancing quality of life. Always consult with an experienced neurosurgeon and multidisciplinary team for optimal outcomes.
What is the Success Rate for Deep brain stimulation (DBS)?
The success rate for Deep Brain Stimulation (DBS) depends on the condition being treated, the patient's overall health, and the accuracy of the procedure. Here’s an overview of success rates for the most common conditions treated with DBS:
1. Parkinson’s Disease
- Symptom Reduction: DBS significantly reduces motor symptoms such as tremors, rigidity, and dyskinesia in 70–90% of patients.
- Medication Reduction: Many patients experience a substantial reduction in the need for Parkinson's medications, lowering side effects such as motor fluctuations.
- Improved Quality of Life: Studies show that DBS improves the overall quality of life in 80% of appropriately selected Parkinson’s patients.
2. Essential Tremor
- Tremor Control: DBS provides 80–90% reduction in tremors, particularly in the hands, enabling better daily functioning.
- Sustained Effects: Tremor control is long-lasting, with benefits persisting for many years.
3. Dystonia
- Symptom Improvement: Approximately 60–80% of patients with dystonia experience significant improvement in muscle contractions and posture.
- Better Outcomes: Patients with early-onset dystonia generally have better outcomes than those with secondary or acquired dystonia.
4. Obsessive-Compulsive Disorder (OCD)
- Symptom Reduction: About 50–60% of patients with treatment-resistant OCD experience significant improvement in symptoms.
- Emotional Well-being: DBS can improve mood, reduce anxiety, and enhance overall mental health.
5. Epilepsy
- Seizure Reduction: Patients often experience a 50–70% reduction in seizure frequency over time.
- Improved Control: DBS is particularly effective for those with drug-resistant epilepsy.
Factors Affecting Success
- Patient Selection: Success rates are higher in carefully selected patients with clear indications for DBS.
- Surgical Accuracy: Precise placement of the electrodes in the target brain area is critical.
- Device Programming: Ongoing adjustments by a skilled neurologist significantly influence outcomes.
Long-Term Effectiveness
- DBS is a durable treatment, with most patients experiencing long-lasting symptom relief. However, as the underlying conditions progress (e.g., Parkinson’s), adjustments may be needed to maintain effectiveness.
Risks and Considerations
While the success rates are high, some patients may experience complications such as infections, hardware issues, or side effects like speech or mood changes. A skilled multidisciplinary team is essential to optimize outcomes and manage potential risks.Overall, DBS offers substantial and sustained benefits for appropriately selected patients, significantly enhancing their quality of life.
What Question Should Ask for Deep brain stimulation (DBS)?
-
Are you the board-certified best neurosurgeon in India?
Yes, confirm your neurosurgeon is board-certified, experienced in DBS, and affiliated with reputable institutions specializing in movement disorders and neuromodulation. -
How many years of experience do you have in this field?
Experienced DBS surgeons typically have 10–20 years in neurosurgery and specialized training in DBS. -
How many surgeries are you doing every day?
DBS is a highly specialized procedure, so most surgeons perform 1–2 surgeries per week or about 50–100 annually. -
How much does Deep Brain Stimulation Surgery (DBS) Cost in India?
The cost ranges from ₹7,00,000 to ₹20,00,000 ($8,500–$25,000), including pre-operative evaluations, surgery, and follow-ups. -
Which are the best hospitals for DBS surgery in Delhi?
Top hospitals include AIIMS (Delhi), Medanta, Max Super Specialty Hospital, and Apollo Hospitals. -
Does your hospital certify to perform these types of surgery?
Ensure the hospital is equipped with advanced neurosurgical infrastructure, such as intraoperative imaging and stereotactic systems. -
Am I a good patient for this procedure?
Candidates typically include patients with Parkinson’s disease, essential tremor, or dystonia who have not responded well to medication. -
What are the success rates and how long will recovery take?
Success rates are about 70–90% for symptom improvement, with initial recovery taking 2–4 weeks and system programming occurring over months. -
What treatment plan do you recommend and why?
DBS is recommended for managing motor symptoms of movement disorders. Other options like medication adjustments or physical therapy may also be considered. -
What are the advantages and disadvantages of DBS surgery?
Advantages: Significant symptom relief, reversible, adjustable settings.
Disadvantages: Risks of infection, bleeding, device malfunction, and potential side effects like speech or cognitive changes. -
What are the costs involved in DBS surgery?
Costs include pre-surgical evaluations, surgical fees, hospital stay, hardware (neurostimulator and electrodes), and follow-ups. -
How much does deep brain stimulation cost in Delhi?
DBS costs in Delhi range from ₹10,00,000 to ₹18,00,000 ($12,000–$22,000), depending on the hospital and technology used. -
How can I prevent damage to the DBS system?
Avoid vigorous physical activities, direct impact to the implant site, and exposure to strong electromagnetic fields. -
What benefits can I expect from DBS? How long do the benefits from DBS last?
Benefits include reduced tremors, rigidity, and improved quality of life. Effects may last for many years but depend on disease progression. -
After DBS, can I have other types of surgery?
Yes, but inform all healthcare providers about the implant. Precautions are necessary for surgeries involving electromagnetic equipment. -
Can I have a pacemaker or an implantable cardioverter defibrillator (ICD) with DBS?
Yes, but it requires careful coordination between the cardiologist and neurosurgeon to avoid interference. -
Can I have diathermy with DBS?
No, diathermy is contraindicated as it can damage the DBS system or surrounding tissue. -
Can I use a hyperbaric chamber with DBS?
Generally safe, but consult your neurosurgeon as extreme pressure changes may affect the device. -
If I get cancer, can I have radiation therapy with DBS?
Yes, but shielding and careful planning are required to avoid damage to the device. -
Can I use a transcutaneous electrical nerve stimulation (TENS) unit with DBS?
Use with caution as it may interfere with the neurostimulator. Consult your doctor for safe settings. -
What happens if the neurostimulator stops working?
Symptoms may return. Emergency evaluation and reprogramming or replacement are required. -
How long will the neurostimulator battery last?
Batteries typically last 3–5 years for non-rechargeable devices and up to 15 years for rechargeable ones. -
What happens when my neurostimulator is ready to be replaced?
Replacement involves a minor surgery to replace the battery or entire neurostimulator. -
How long do I have to stay in and outside the hospital?
Hospital stay is 3–5 days, with additional recovery at home for 2–4 weeks. -
What are the risk factors for this type of surgery?
Risks include infection, hemorrhage, hardware-related complications, and potential neurological side effects. -
When can I go for normal activities, including exercise?
Light activities can resume within 2–4 weeks. Vigorous activities require 6–8 weeks or clearance from your doctor. -
Do I have stitches, staples, and/or bandages?
Yes, surgical incisions are closed with stitches or staples, typically removed after 10–14 days. -
Do I have a scar or other permanent effects from the surgery?
Small scars will remain at the implant and incision sites. -
Do I need to go to another surgery in the future?
Additional surgeries may be required for battery replacement or hardware issues. -
Do I need any follow-up appointments or tests after my surgery?
Yes, follow-ups include neurostimulator programming and periodic evaluations to monitor device functionality and symptom improvement.
Top Doctors
Top Hospitals
DEEP BRAIN STIMULATION COST IN INDIA
Duration of Treatment
usually takes 4 to 5 hours.
Days of Stay
usually 3 to 5 days in the hospital and 30 days outside the hospital.
Anesthesia
Local and General Anesthesia.
Cost
22,000 to 28,000 USD
How much does Deep Brain Stimulation Surgery (DBS) Cost in India?
"Looking for Deep Brain Stimulation Surgery Cost in India or Best Neurosurgeon at an affordable cost in different cities like Delhi, Mumbai, Chennai, Kolkata, and Bangalore? Here, we answer the question and explain how to choose the best neuro hospital list for better results.
We have also shortlisted the list of best top Hospitals and Surgeons on the basis of Hospital accreditations, experience & qualification of surgeons, success rates of procedures, and patient testimonials.
- Deep Brain Stimulation Surgery Cost in India : Starting from 22,000 to 28,000 USD
- Hotel Cost Near Hospital - starting from 18 to 50 USD ( as per hotel services)
- Food Cost - starting from 20 to 30 USD (per day )
- Miscellaneous cost - 20 USD (per day)
- It's an only rough estimate, final treatment will plan after the fresh evaluation reports.
- Deep Brain Stimulation Surgery Cost in India can vary as per the diagnosis, patient conditions, surgeon experience, Implant quality, hospital facilities, and city.
- To make an appointment, learn more about brian, read below information, or call / WhatsApp/ Viber - our experts to answer at +91 9582708782. Still, have questions? SUBMIT ENQUIRY
Who is the Top Best NeuroSurgeon in India?
- Dr. Bipin Walia
- Dr. Rana Patir
- Dr. Anil Kumar Kansa
- Dr. Vikas Gupta
- Dr. Aditya Gupta
- Dr. Sunit Mediratta
- Dr. Rahul Gupta
- Dr. Arun Saroha
- Dr. Anandh Balasubramaniam
- Dr. Shibu Vasudevan Pillai
Which is the Best DBS Hospital in India?
- ARTEMIS HOSPITAL
- MANIPAL HOSPITAL
- BLK HOSPITAL
- APOLLO HOSPITAL
- FORTIS HOSPITAL
- MAX HOSPITAL
- MEDANTA HOSPITAL
- YASHODHA HOSPITAL
- GLOBAL HOSPITAL
- NARAYANA HOSPITAL
Why did you choose Peace Medical Tourism?
We are one of the best healthcare services providers with more than 10 years of experience in providing the best treatment at an affordable cost and guide our international patients to choose the top destination as per patient's budget and treatment.
- Comprehensive and 100% transparency.
- Help to Choose the Best Option for Treatment.
- Very highly skilled Neurosurgeon in India team.
- World-class technology for surgery.
- The high success rate of procedures with international standards.
- Affordable Cost of DBS surgery.
What is Deep Brain Stimulation?
Deep brain stimulation (DBS) is a surgical procedure that involves implanting an electrode device called a brain pacemaker, to send electrical impulses to the areas of the brain that control movement, pain, mood, weight, and awakening. Deep brain stimulation is used to treat, Essential tremors, Parkinson's disease, Tourette syndrome, Chronic Pain, Dystonia, and Epilepsy.
Types of Deep Brain Stimulation:-
- Subthalamic DBS
- Globus pallidus DBS
- Thalamic DBS
- Pedunculopontine nucleus DBS
Still, have questions? SUBMIT ENQUIRY
symptoms
What are the Signs and Symptoms of Deep brain stimulation (DBS) surgery?
- Essential tremor
- Multiple sclerosis
- Dystonia
- Psychiatric conditions
- Alzheimer’s disease
risk factors
What are the risk factors of Deep brain stimulation (DBS) surgery?
- Bleeding in the brain
- Stroke
- Brain swelling
- Vision and speech defect
- Infection
- Coma
- Breathing problems
- Nausea
- Heart problems
- Seizures
preparation
How to Prepare yourself for Deep brain stimulation (DBS) surgery?
- First, you have to choose the Best neuro hospitals in India or abroad and a top neurosurgeon at an affordable cost for better results.
- The patient is required to go for PSC ( Pre-surgery check-up ) to do some blood test, ECG and ECH for Cardiac check-up and urine tests to know he /she is fit for surgery or not.
- Comprehensive Assessment: The patient undergoes neurological evaluations, imaging (MRI or CT scans), and psychological assessments to confirm suitability for DBS.
- Identifying Target Areas: Based on the disorder, specific brain areas such as the subthalamic nucleus (STN), globus pallidus interna (GPi), or thalamus are selected for stimulation.
- Before the operation, you’ll be asked to sign a consent form, which gives the surgeon permission to carry out the treatment.
- The doctor should be informed about any medication that the patient may be taking.
- The patient is admitted to the hospital on the same days before the procedures and advised to remain empty stomach/Fasting.
- Thinners medicines have to stop before ten days of surgery.
procedure
What is the Procedure for Deep brain stimulation (DBS) surgery?
To identify the diagnosis doctor advised to go for complete evolution - usually, blood investigation, (CT) scans, magnetic resonance (MRI) imaging for brain-imaging studies, angiography (imaging the brain's blood vessels), and ventriculography (imaging the brain's ventricles). Before surgery, the surgeon and anesthesia will guide you about the benefits and risk factors of Deep brain stimulation (DBS) surgery.
Step 1 – Anesthesia: Deep brain stimulation (DBS) surgery takes 4 to 5 hours depending upon the procedures by giving local or general anesthesia to relieve pain.
Step 2 – The incision: Deep brain stimulation surgery is usually done in two stages.
- First Stage (Brain surgery) - The patient will go under local anesthesia. The patient’s head is placed in a rigid frame using small screws is called frame-based stereotaxis. And the neurosurgeon makes a small hole into the skull to insert a thin wire lead and will place in a particular part of the brain. A wire goes under the skin and pulse generator implanted near the collarbone.
Surgical Preparation
- Stereotactic Frame Placement: A lightweight frame is attached to the patient’s head under local anesthesia to provide precise coordinates for targeting the brain.
- Imaging for Target Localization: An MRI or CT scan is performed to map the brain and identify the exact location of the target area.
mplanting the Electrodes
- Procedure Type: Usually performed under local anesthesia so the patient can provide feedback to assess symptom improvement during surgery.
- Drilling Small Holes: Small holes are drilled into the skull to access the brain.
- Electrode Placement: Thin, insulated wires (electrodes) are inserted into the target area of the brain using a stereotactic system for precision.
- Intraoperative Testing: Temporary stimulation is performed to confirm the electrodes are correctly placed by observing symptom reduction or monitoring brain responses.
Implanting the Neurostimulator
- General Anesthesia: Once the electrodes are placed, the patient is typically put under general anesthesia.
- Pulse Generator Placement: A small device called a neurostimulator (similar to a pacemaker) is implanted under the skin, usually in the chest or abdomen.
- Connecting Wires: Leads from the brain electrodes are tunneled under the skin and connected to the neurostimulator.
- Second Stage (Chest wall surgery) - The patient will go under General anesthesia. A small incision is made below the collarbone. A wire goes under the skin and pulse generator implanted near the collarbone. This extension of thin wire connects the electrode to the neurostimulator and is programmed to send continuous electrical pulses to your brain.
Step 3 – Closing the incisions: The neurosurgeon flaps the skin after the surgery with the help of Sutures, skin adhesives, tapes or clips that close the skin incisions.
post procedure
What is the Post care for Deep brain stimulation (DBS)?
The doctor will give complete information about post care of surgery, regarding recovery; proper caring of incisions, taking medications, and managing. Stitches or staples will be removed after a few days of surgery. The batteries of the neurostimulator need to be changed in 3 to 5 years.
Post-Surgical Programming
- Device Activation: A few weeks after surgery, the neurostimulator is activated and programmed by a neurologist or movement disorder specialist.
- Adjusting Settings: The device’s electrical pulses are fine-tuned to optimize symptom control while minimizing side effects.
Additional Considerations
- Adjustable and Reversible: DBS does not destroy brain tissue, and the settings can be modified or turned off if necessary.
- Battery Replacement: Depending on the device type, the neurostimulator battery may need replacement every 3–5 years (non-rechargeable) or recharging at regular intervals (rechargeable).
his step-by-step procedure ensures a personalized and precise approach to improving symptoms and enhancing quality of life. Always consult with an experienced neurosurgeon and multidisciplinary team for optimal outcomes.
success rate
What is the Success Rate for Deep brain stimulation (DBS)?
The success rate for Deep Brain Stimulation (DBS) depends on the condition being treated, the patient's overall health, and the accuracy of the procedure. Here’s an overview of success rates for the most common conditions treated with DBS:
1. Parkinson’s Disease
- Symptom Reduction: DBS significantly reduces motor symptoms such as tremors, rigidity, and dyskinesia in 70–90% of patients.
- Medication Reduction: Many patients experience a substantial reduction in the need for Parkinson's medications, lowering side effects such as motor fluctuations.
- Improved Quality of Life: Studies show that DBS improves the overall quality of life in 80% of appropriately selected Parkinson’s patients.
2. Essential Tremor
- Tremor Control: DBS provides 80–90% reduction in tremors, particularly in the hands, enabling better daily functioning.
- Sustained Effects: Tremor control is long-lasting, with benefits persisting for many years.
3. Dystonia
- Symptom Improvement: Approximately 60–80% of patients with dystonia experience significant improvement in muscle contractions and posture.
- Better Outcomes: Patients with early-onset dystonia generally have better outcomes than those with secondary or acquired dystonia.
4. Obsessive-Compulsive Disorder (OCD)
- Symptom Reduction: About 50–60% of patients with treatment-resistant OCD experience significant improvement in symptoms.
- Emotional Well-being: DBS can improve mood, reduce anxiety, and enhance overall mental health.
5. Epilepsy
- Seizure Reduction: Patients often experience a 50–70% reduction in seizure frequency over time.
- Improved Control: DBS is particularly effective for those with drug-resistant epilepsy.
Factors Affecting Success
- Patient Selection: Success rates are higher in carefully selected patients with clear indications for DBS.
- Surgical Accuracy: Precise placement of the electrodes in the target brain area is critical.
- Device Programming: Ongoing adjustments by a skilled neurologist significantly influence outcomes.
Long-Term Effectiveness
- DBS is a durable treatment, with most patients experiencing long-lasting symptom relief. However, as the underlying conditions progress (e.g., Parkinson’s), adjustments may be needed to maintain effectiveness.
Risks and Considerations
While the success rates are high, some patients may experience complications such as infections, hardware issues, or side effects like speech or mood changes. A skilled multidisciplinary team is essential to optimize outcomes and manage potential risks.Overall, DBS offers substantial and sustained benefits for appropriately selected patients, significantly enhancing their quality of life.
faqs from doctor
What Question Should Ask for Deep brain stimulation (DBS)?
-
Are you the board-certified best neurosurgeon in India?
Yes, confirm your neurosurgeon is board-certified, experienced in DBS, and affiliated with reputable institutions specializing in movement disorders and neuromodulation. -
How many years of experience do you have in this field?
Experienced DBS surgeons typically have 10–20 years in neurosurgery and specialized training in DBS. -
How many surgeries are you doing every day?
DBS is a highly specialized procedure, so most surgeons perform 1–2 surgeries per week or about 50–100 annually. -
How much does Deep Brain Stimulation Surgery (DBS) Cost in India?
The cost ranges from ₹7,00,000 to ₹20,00,000 ($8,500–$25,000), including pre-operative evaluations, surgery, and follow-ups. -
Which are the best hospitals for DBS surgery in Delhi?
Top hospitals include AIIMS (Delhi), Medanta, Max Super Specialty Hospital, and Apollo Hospitals. -
Does your hospital certify to perform these types of surgery?
Ensure the hospital is equipped with advanced neurosurgical infrastructure, such as intraoperative imaging and stereotactic systems. -
Am I a good patient for this procedure?
Candidates typically include patients with Parkinson’s disease, essential tremor, or dystonia who have not responded well to medication. -
What are the success rates and how long will recovery take?
Success rates are about 70–90% for symptom improvement, with initial recovery taking 2–4 weeks and system programming occurring over months. -
What treatment plan do you recommend and why?
DBS is recommended for managing motor symptoms of movement disorders. Other options like medication adjustments or physical therapy may also be considered. -
What are the advantages and disadvantages of DBS surgery?
Advantages: Significant symptom relief, reversible, adjustable settings.
Disadvantages: Risks of infection, bleeding, device malfunction, and potential side effects like speech or cognitive changes. -
What are the costs involved in DBS surgery?
Costs include pre-surgical evaluations, surgical fees, hospital stay, hardware (neurostimulator and electrodes), and follow-ups. -
How much does deep brain stimulation cost in Delhi?
DBS costs in Delhi range from ₹10,00,000 to ₹18,00,000 ($12,000–$22,000), depending on the hospital and technology used. -
How can I prevent damage to the DBS system?
Avoid vigorous physical activities, direct impact to the implant site, and exposure to strong electromagnetic fields. -
What benefits can I expect from DBS? How long do the benefits from DBS last?
Benefits include reduced tremors, rigidity, and improved quality of life. Effects may last for many years but depend on disease progression. -
After DBS, can I have other types of surgery?
Yes, but inform all healthcare providers about the implant. Precautions are necessary for surgeries involving electromagnetic equipment. -
Can I have a pacemaker or an implantable cardioverter defibrillator (ICD) with DBS?
Yes, but it requires careful coordination between the cardiologist and neurosurgeon to avoid interference. -
Can I have diathermy with DBS?
No, diathermy is contraindicated as it can damage the DBS system or surrounding tissue. -
Can I use a hyperbaric chamber with DBS?
Generally safe, but consult your neurosurgeon as extreme pressure changes may affect the device. -
If I get cancer, can I have radiation therapy with DBS?
Yes, but shielding and careful planning are required to avoid damage to the device. -
Can I use a transcutaneous electrical nerve stimulation (TENS) unit with DBS?
Use with caution as it may interfere with the neurostimulator. Consult your doctor for safe settings. -
What happens if the neurostimulator stops working?
Symptoms may return. Emergency evaluation and reprogramming or replacement are required. -
How long will the neurostimulator battery last?
Batteries typically last 3–5 years for non-rechargeable devices and up to 15 years for rechargeable ones. -
What happens when my neurostimulator is ready to be replaced?
Replacement involves a minor surgery to replace the battery or entire neurostimulator. -
How long do I have to stay in and outside the hospital?
Hospital stay is 3–5 days, with additional recovery at home for 2–4 weeks. -
What are the risk factors for this type of surgery?
Risks include infection, hemorrhage, hardware-related complications, and potential neurological side effects. -
When can I go for normal activities, including exercise?
Light activities can resume within 2–4 weeks. Vigorous activities require 6–8 weeks or clearance from your doctor. -
Do I have stitches, staples, and/or bandages?
Yes, surgical incisions are closed with stitches or staples, typically removed after 10–14 days. -
Do I have a scar or other permanent effects from the surgery?
Small scars will remain at the implant and incision sites. -
Do I need to go to another surgery in the future?
Additional surgeries may be required for battery replacement or hardware issues. -
Do I need any follow-up appointments or tests after my surgery?
Yes, follow-ups include neurostimulator programming and periodic evaluations to monitor device functionality and symptom improvement.